Professionals
Welcome to the Professionals pages

Welcome to the LSCP Professionals pages. Here you will find key information, resources and links to support you in work to safeguard children.
Visit our Partnership Learning tab to find out about courses and learning events available to you
Have you seen the latest LSCP Safeguarding Briefing?
LSCP Family Help Continuum of Need (2024-25)
This document has been updated from October 2024 in line with the DfE Families First Pathfinder which sets out our approach to keeping children safe and protected, and underpins our local vision to provide the right support at the right time for children and families in Lewisham, at the earliest opportunity. This document is aligned to the London Safeguarding Children: Threshold Document: Continuum of Help and Support; however our language and terminology in Lewisham has been reframed as we develop our Family Help offer.

In Lewisham we know that the majority of children, young people and their families can be supported through a range of universal services. These services include education, early years, health, housing, and services provided by voluntary organisations. These services include education, early
years, health, housing, and services provided by voluntary organisations. However, some children have more complex needs and may require access to Family Help to support them. We want to ensure that we provide the right help and support for families which is led by the presenting need and not a prescribed framework. We understand the need to be flexible and have adaptable responses to how we with work with families.
This document provides an overview to support all professionals and agencies who work with children and young people, from or in the Borough of Lewisham, to identify when help or protection is needed through families lives. Its purpose is to develop shared guidance and understanding that sets out the local partnership arrangements for the planning and provision of services.
The document should be read alongside statutory guidance outlined in the London Safeguarding Children Partnership Threshold - Continuum of Need Matrix to consider specific indicators.
NB. Agencies in the London Borough of Lewisham should also comply with additional LSCP local protocols and practice guidance that are published on the LSCP website.
LSCP Family Help Continuum of Need 2024-2025
LSCP Family Help Continuum- Key Summary 2024
Prevention and Family Advice
Our vision for our Prevention and Family Advice offer is for children and young people in Lewisham to thrive, reaching their full potential and able to take full advantage of the opportunities available to them in Lewisham, London and beyond.'
Prevention and Family Advice offer describes support available to children, young people and families up to the level of statutory or specialist intervention. It is there to support from pre-natal stages up to the age of 18 years (25 years for those with SEND). It includes information and advice, universal services, open access services and more tailored support for children, young people, and families.
‘Working together to safeguard children’ (2023) is the statutory guidance which details the vital role of effective early help intervention for children at risk of poorer outcomes. It emphasises that all agencies have a collective responsibility, to identify, assess and provide effective prevention and advice services. Our LSCP Family Help Continuum of Need Document will help you assess the level of support needed or risks present. Professionals should refer to the continuum of need document before making a FFCP request.
Within our Prevention and Family Advice offer there are both information and advice services. These services work together, ensuring the most relevant and focused plans and interventions are in place:
- Family Information are services that all children and families can access (for example, Family Hubs, Children Centres, GPs, Schools, Early Years, Community organisations etc.)
- Family Advice are services for children and families that have multiple needs which require a multi-agency intervention (for example, Family Thrive). The Families First Contact Point (FFCP) is the single point of entry for referrals to Lewisham’s Family Thrive Service.
Family Thrive
Family Thrive is a consent based Family Advice Service.
Family Thrive works with families who have children aged 0 to 18 years, (and up to 25 years for SEND) who may require tailored parenting support to help them be happier and healthier. We work closely with schools and other professionals with consent. Consent from the parents/carers must be gained at the point of referral.
Family Practitioners undertake a Family Advice Record & Plan, and develop outcome-focused plans in line with Signs of Safety and in a way that promotes holistic and family led planning
The Family Practitioner is the lead professional and work alongside partner agencies as part of the multidisciplinary Team Around the Family and provide tailored parenting support and undertake direct work with children and young people.
Parenting Support
Instances where there is low level or emerging concerns might result in referrals to the Prevention & Family Advice service for tailored parenting support from the Family Thrive Service. Skilled Family Practitioners will undertake focused family based interventions for a fixed period of time working with parents to sustain positive parenting practices and ensure all appropriate support needs are provided.
Parents can also attend any of Lewisham’s Family Hubs for support, advice and access to parenting support such as:
Family Navigators
You can talk to one of our Family Navigators who are based in our Family Hubs offering free, confidential and non-judgmental support if you are a parent or carer living in Lewisham.
Owl Babies Course
During this course we share ideas, talk about the challenges of being a parent, support mental and emotional wellbeing using Five to Thrive, Nature and the outdoor environment.
Baby Massage
Our baby massage courses aim to support your bond with your baby through easy to learn, gentle and positive movements whilst enjoying relaxing and special one to one time together.
Triple P for Babies
Triple P for Baby programme aims to prepare parents for a positive transition to parenthood and the first year with baby, promoting sensitive and responsive care in the perinatal period
Staying Healthy
At Lewisham Family Hubs Families can sign up for and collect FREE Vitamin D and attend Weaning and Healthy Eating Sessions and Courses.
These include:
- Starting Solids
- Portion Sizes
- Fussy Eating
Visit www.lewishamfamilyhubs.org for more information, timetables and details of Family Hub locations
Non-Violent Resistance-Informed Parenting Programme
- The programme is aimed at parents and carers of pre-teen children (aged 8 years and over) experiencing challenging/violent and extreme behaviours.
- NVR is a concept that draws inspiration from those who have sought to bring about changes in society in a non violent manner.
- The programme offers a series of tools and techniques to support parents and carers of children and young people who display challenging attitudes and behaviours.
- Parents are guided through a set of core principles based on the idea of carefully planned actions to help support the management of challenging behaviour.
Triple P (Positive Parenting Programme)
- Positive Parenting Programme, is a broad-based parenting programme for parents and carers of children aged between 2-10yrs who are struggling to manage aspects of their children’s behaviour.
- The programme is 6 to 8 weeks long made up of 4 mandatory classroom sessions between 2 and 4 individualised 1:1 sessions.
Children Overcoming Domestic Abuse (CODA)
- CODA is a twelve-week recovery intervention for mothers and their children who have experienced domestic abuse. We are currently delivering to children in Years 3 and 4.
- Running concurrently, CODA provides two-hour sessions for mothers and their children on a weekly basis. Each week covers a specific theme and programmes are divided into age appropriate groups. Note: siblings cannot access the same group.
- CODA seeks to support the recovery process and aims to:
- Validate the children’s experiences
- Reduce the self-blame that is commonly associated with children experiencing abuse
- Develop a child-appropriate safety plan
- Manage emotions appropriately
- Enhance the mother-child relationship
- Enable both the mother and child to heal together
The Juniper Programme
- The Juniper Programme has the same aims as the CODA Programme but is delivered to children under the age of four years and the adult survivor.
More information on all Family Hubs service can be found at www.lewishamfamilyhubs.org.uk.
Families First Contact Point (FFCP)
What is the FFCP?
The Families First Contact Point (FFCP) (formerly known as the Multi-Agency Safeguarding Hub - MASH) provides a single point of access to the services that help keep children safe. It is a multi-agency team made up of representatives from a range of services that provide advice, support and protection as needed. These services include:
Family First Contact Point (FFCP)
Allegations Against Professionals (LADO)
Making a referral to the Local Authority Designated Officer and Possible Outcomes
The LADO (Local Authority Designated Officer) provides advice and guidance to employers and other individuals/organisations who have concerns relating to an adult who works with children and young people (including volunteers, agency staff and foster carers) or who is in a position of authority and having regular contact with children (e.g. religious leaders or school governors).
There may be concerns about workers who have:
- behaved in a way that has harmed or may have harmed a child
- possibly committed a criminal offence against or related to a child
- Behaved towards a child or children in a way that indicates they may pose a risk of harm to children;
- behaved towards a child, or behaved in other ways that suggests they may be unsuitable to work with children
What should be referred to the LADO?
Any concern that meets the criteria above should be referred. Initially it may be unclear how serious the allegation is. If there's any doubt, the LADO or the designated safeguarding lead person in your agency should be contacted for advice.
What the LADO does:
The first step will be to offer an initial consultation about the concern. This may consist of advice and guidance regarding the most appropriate way of managing the allegation. The LADO will:
- help establish what the 'next steps' should be in terms of investigating the matter further
- liaise with the police and other agencies, and arrange for an allegations meeting to be held if required; if the case is complex there may be a series of meetings
- monitor and maintain an overview of cases which meet threshold to ensure they're dealt with as quickly as possible, consistent with a thorough and fair process
- ensure child protection procedures are initiated where the child is considered to be at risk of significant harm
- ensure the appropriate agencies are involved in the investigation
- ensure advice is provided in relation to the adults remaining in post over the course of the investigation
- ensure issues of sharing information with parents and other relevant individuals are considered
- assist an employer in decisions about a person's suitability to remain in the children's workforce, and whether a referral should be made to the Disclosure and Barring Service (DBS) or the appropriate regulatory or professional body
- In cases where the adult is unaware of the concern or allegation, it may not be appropriate to tell them immediately and may prejudice a potential police investigation. The LADO will provide advice.
Outcomes
The outcomes from a LADO referral may include:
- finding that the allegation is malicious
- finding that the allegation is unsubstantiated
- finding that the allegation is substantiated
- finding that the allegation is false
- finding that the allegation is unfounded
- internal investigation by the employer including consideration of disciplinary procedures
- a police investigation
- police prosecution
- Where the adult is reinstated there may be recommendations in relation to additional support, monitoring or training.
- Where an individual is dismissed from their post, a referral must be made to the DBS which makes decisions on whether individuals should be barred from working with children.
- Compromise agreements are not an acceptable resolution to a concern, and even if someone resigns it should not prevent a full and thorough investigation into the matter.
LADO Procedure & Protocol - 2023
To make a referral to the Local Authority Designated Officer (LADO), please email a LADO Contact & Referral Form to LewishamLADO@Lewisham.gov.uk.
Named Lewisham LADO:
Eleanor Hargadon-Lowe, London Borough of Lewisham, 1st Floor Laurence House, 1 Catford Road, SE6 4RU
There is also a Deputy LADO system, as such you may speak with and be supported by a member of the team.
LADO Voicemail service: 020 8314 7280. Please note this is a manned voicemail, so please leave a clear message and the LADO or Deputy LADO will respond to you as soon as possible within 24 hours.
LADO Annual Reports
LADO Annual Report 2023-2024
LADO Annual Report 2022-2023
Useful Links
London Safeguarding Children Procedures
London Safeguarding Children's Partnership
Working Together to Safeguard Children 2023
Keeping Children Safe in Education 2023
Child Not Brought to Appointments
The following animation is aimed at raising awareness about the consequences of missing appointments and to ensure that children and adults get the medical care that they need. This is a powerful reminder that children do not take themselves to appointments, and for practitioners to reflect on the impact of missed appointments on a child's wellbeing. With thanks to Nottingham City CCG & Safeguarding Children Partnership.
Definitions:
Child Not Brought (CNB): Child was not brought to the appointment without cancellation.
Did Not Attend (DNA): Did not attend appointment without cancellation
No Access Visit (NAV): Not available at home to be seen for appointment.
Background
It is recognised that many children miss appointments in hospital and community settings, and are not available at home to be seen by staff working in different agencies.
Many Serious Child Safeguarding Practice Reviews (Serious Case Reviews) / Homicide Reviews both nationally and regionally have featured CNB, DNA and NAV as a precursor to serious child abuse and child death.
Key principles for Practice
Organisations
- All agencies should have a policy and local guidance for managing CNB, DNA and NAVs which underpins both process and practice and reflects the differing needs of children and their families.
- Services provided should be child and young person friendly and work in partnership with parents and other practitioners.
Practitioners
- Practitioners should be child focussed and consider children and young people even when the CNB / DNA / NAV relates to the parent/carer, particularly when mental health or problematic substance misuse is featured.
- Practitioners should ensure they are appropriately trained in the identification of child maltreatment to ensure effective judgements are made as to whether the child or young person’s health and development are subject to impairment.
- Develop robust communication links with parents and other professionals or agencies working with the child and ensure that any outcome or consequence for the child or young person is explained.
- Know when and with whom to share information when there are concerns about a child or young person’s welfare and where to get advice.
- Document assessments, analysis, communications and actions taken in the child / young person or parent / carer record as relevant.
- Parents / Carers may disengage with any agencies caring for themselves or their children.
- Remember disengagement is a key risk factor for children and families and may be a precursor to something more serious happening.
Managing CNB/DNA/NAV
Assessment
- Following CNB / DNA / NAV the responsibility for any assessment of the situation rests with the practitioner to whom the child has been referred in conjunction with the referrer (Laming 2003).
- Consider the needs of the child and the parents / carers capacity to meet those needs.
- Consider environmental context of the child’s situation.
- Identify whether intervention is required to secure a child’s welfare.
Communication
- Verbal / written communication with the parents / referrer needs to outline consequence of CNB / DNA / NAV on the child.
- Where there are clear child protection concerns, discuss these with your line manager and make a referral to the Multi-Agency Safeguarding Hub (MASH) mashagency@lewisham.gov.uk in accordance with Lewisham’s procedures.
- Where there are concerns relating to children, information should be shared with the Line Manager, Named or Designated Safeguarding Lead / Lead Professional or other agency working with the family who can add to the information sharing process.
Record Keeping
- The content of discussions should be clearly documented along with any actions and outcomes in the child or parent / carer record.
- Analysis and conclusion should also be documented ensuring that any referral letters and context of previous records have been considered.
Action
- Consider arranging another appointment, check addresses and other details for accuracy.
- Ensure parents / carers are informed about the consequence(s) of further non-attendance for the child / young person and with whom information will be shared with should there be further CNB / DNA / NAV.
- Repeated CNB / DNA / NAV should result in a Team Around the Family (TAF) meeting to agree the best course of action.
- Unless there is a concern that a child / young person is likely to suffer significant harm then a referral should not be made to MASH until it is established the TAF has not worked. The referral will need to show what work has been attempted, by whom, and what is expected a referral to MASH will achieve.
- An immediate referral to MASH should be made if it is established urgent medical attention has not been sought or delayed for a child or young person by a parent / carer.
Audit
- Agencies should find ways to collect information in respect of CNB / DNA / NAV to increase the uptake of services in order to safeguard children and young people and improve their outcomes.
Audit Suggestions
- Number of services CNB / DNA / NAVs under the age of 18 and include the outcome.
- Number of service CNB / DNA for mental health, drug and alcohol services including outcomes of the CNB / DNA.
- Number of NAVs including outcome of no access (all services).
- GP’s should audit outcomes of CNB / DNA / NAV and consider the consequence of non-engagement in order to work with families to improve engagement.
Additional Policies
L&G NHS Trust – Child Was Not Brought / No Access Visit Policy December 2019
Useful Websites
www.london safeguarding children partnership.gov.uk
www.everychildmatters.gov.uk
Child Protection Conferences
Reports
The London Borough of Lewisham Multi-Agency Child Protection Conference Report Template was introduced in February 2022.
ALL professional agencies must complete this report, even if they are unable to attend but are invited. This must be sent to the Quality Improvement Business Support Team (QISBusinessSupport@lewisham.gov.uk) within the following timescales:
- Initial Child Protection Conference – 2 working days before
- Review Child Protection Conference - 5 working days before
These reports must be shared with the families before the meeting – there should not be any information that the family do not know that will be shared in the meeting. If there is confidential information that cannot be shared with the family in the conference due to concerns that this will increase risk to children, then please alert the Chair to this before the meeting.
Structure of the Conference
The Conference is chaired by a Child Protection Chairperson, who is a qualified and experienced social work professional. Their responsibility in the meeting is to make decisions in respect of the level of risk faced by a child, and create a multi-agency plan that aims to keep the child safe.
The chair will endeavour to gather information (not already provided in the reports) and seek to focus on the key areas of risk/ harm to the child, and any examples or times where the risk has been managed and the child kept safe (this is called existing safety).
The Chair will speak with everyone in the conference to gather their views and analysis, as well as recommendation (see below).
Participation in the Conference
All relevant professionals who are involved with a child or their family are requested to attend a Child Protection Conference. The focus in the meeting will be around analysis of the harm and safety and what plan needs to be in place to address the key areas of danger and risk.
It is really important for professionals to keep their summaries brief in conference. If they have completed and shared their reports in advance of the conference meeting then this should mean they do not need to repeat the information in their report (the ‘detail’). The Conferences need to be a balance of pulling out the pertinent details about risk and existing examples of safety, and creating a multi-agency plan that is likely to keep the child safe. It is not meant to be an opportunity to share an exhaustive bullet point list of what is working well, and what is not.
Scaling, Recommendations and Categories
We use the Signs of Safety model in our conferences. One of the tools within this model is the scaling. We use a ‘Safety scale’ which means when scoring, we are considering how ‘safe’ the child is on a scale of 0-10. 10 is that the child is safe, 0 is that they are not (in very basic terms). The Chair should set the parameters of what 0 means and what 10 means to allow scoring to reflect the needs of the family. Professionals who haven’t yet been to a conference, or other social care meeting, can ask for some guidance around scoring, but there is no prescriptive way of doing this. It is for each professional to weight where they consider the child and situation is.
All professionals attending a conference are expected to scale and to make a recommendation in conference about whether a plan is required, and if a Child Protection Plan is recommended, what category that be under.
Categories can cause some anxiety for families and professionals alike. The four categories are Emotional Abuse, Physical Abuse, Sexual Abuse and Neglect. It’s important that the professionals are honest with their recommendation – if the parent has neglected their child’s needs even if unintentionally or due to their own issues, it is still neglect.
Attendance at Core Group Meetings
If a professional is identified as part of the Core Group of professionals around a child, then they are requested (and expected) to attend regular core group meetings every 6 weeks. Again, the focus of these meetings is ideally to share updates and review the efficacy of the plan, focus on the risk and safety for the children in question. Scaling is expected at the end of CGMs but no recommendation is considered necessary.
Further Reading
London Child Protection Procedures, Core Procedures, CP4
Working Together 2023
Child Sexual Abuse (CSA)
Child sexual abuse is defined in Working Together to safeguard children 2023 as:
‘Involves forcing or enticing a child or young person to take part in sexual activities, not necessarily involving a high level of violence, whether or not the child is aware of what is happening. the activities may involve physical contact, including assault by penetration (for example, rape or oral sex) or non-penetrative acts such as masturbation, kissing, rubbing and touching outside of clothing. They may also include non-contact activities, such as involving children in looking at, or in the production of, sexual images, watching sexual activities, encouraging children to behave in sexually inappropriate ways, or grooming a child in preparation for abuse. Sexual abuse can take place online, and technology can be used to facilitate offline abuse. Sexual abuse is not solely perpetrated by adult males. Women can also commit acts of sexual abuse, as can other children.’
Lewisham Child Sexual Abuse (CSA) Pathway
The Lewisham CSA and therapeutic pathway sets out how professionals should respond to concerns, disclosures, or allegations of Child Sexual Abuse.
Signs and Indicators of Child Sexual Abuse +
All professionals need to be confident they have the knowledge and skills to recognise when children might be showing them that something is wrong.
Children may also drop hints and clues that the abuse is happening without revealing it outright.
Children often do not talk about sexual abuse because they think it is their fault or they have been convinced by their abuser that it is normal or a “special secret”.
Children may also be bribed or threatened by their abuser or told they will not be believed.
A child who is being sexually abused may care for their abuser and worry about getting them into trouble.
Different families may use different words for their genital area which may make a disclosure less obvious. It is therefore important to consider the child’s presentation and following signs when a child is speaking about something that may not be clear.
Emotional and behavioural signs may include:
- Avoiding the abuser – the child may dislike or seem afraid of a particular person and try to avoid spending time alone with them;
- Sexually inappropriate behaviour – children who have been abused may behave in sexually inappropriate ways or use sexually explicit language;
- Changes in behaviour – a child may start being aggressive, withdrawn, clingy, have difficulties sleeping, have regular nightmares or start wetting the bed;
- Changes in their mood – feeling irritable and angry, or anything out of the ordinary;
- Changes in eating habits of developing an eating problem;
- Problems at school – an abused child may have difficulty concentrating and learning, and their grades may start to drop;
- Alcohol or drug misuse; and
- Self-harm.
Physical signs may include:
- Bruises;
- Bleeding, discharge, pains or soreness in their genital or anal area;
- Sexually transmitted infections; and
- Pregnancy
Signs of online sexual abuse may include:
- Spending a lot more or a lot less time than usual online, texting, gaming or using social media;·Being distant, upset or angry after using the internet or texting;
- Being secretive about who they’re talking to and what they’re doing online or on their mobile phone;
- Having lots of new phone numbers, texts or email addresses on their mobile phone, laptop or other device.
The Centre of Expertise on Child Sexual Abuse have designed a CSA signs and indicators template to help professionals to gather the signs and indicators of sexual abuse and build a picture of their concerns.
Definitions of Child Sexual Abuse +
Harmful sexual behaviour (HSB)
Harmful sexual behaviour (HSB) is developmentally inappropriate sexual behaviour which is displayed by children and young people and which may be harmful or abusive (derived from Hackett, 2014). It may also be referred to as sexually harmful behaviour or sexualised behaviour.
HSB encompasses a range of behaviour, which can be displayed towards younger children, peers, older children or adults. It is harmful to the children and young people who display it, as well as the people it is directed towards.’ NSPCC
Signs of HSB
Children and young people demonstrate a range of sexual behaviours as they grow up, and this is not always harmful.
Sexualised behaviour sits on a continuum with five stages:
- Appropriate – the type of sexual behaviour that is considered ‘appropriate’ for a particular child depends on their age and level of development; Inappropriate – this may be displayed in isolated incidents, but is generally consensual and acceptable within a peer group;
- Problematic – this may be socially unexpected, developmentally unusual, and impulsive, but have no element of victimisation;
- Abusive – this often involves manipulation, coercion, or lack of consent;
- Violent – this is very intrusive and may have an element of sadism.
It is not always easy to identify HSB; the NSPCC have created a guide of age-appropriate healthy sexual behaviour that should be considered when assessing whether a child’s behaviour is healthy or harmful: https://learning.nspcc.org.uk/media/1659/responding-harmful-sexual-behaviour.pdf
In the borough of Lewisham, multi-agencies aim to work together to provide a specialist service to children and young people who have engaged in harmful sexual behaviour (HSB). This includes harm to other children, young people, and themselves. You can find further information on HSB including the criteria for referrals to the HSB Consultation Panel.
Questions to ask when considering if a child is displaying HSB include
- Is the behaviour unusual for that particular child or young person?
- Have all the children or young people involved freely given consent?
- Are the other children or young people distressed?
- Is there an imbalance of power?
- Is the behaviour excessive, degrading or threatening?
- Is the behaviour occurring in a public or private space?
Child sexual exploitation (CSE) Is defined by the Department of Education as:
‘Child sexual exploitation is a form of child sexual abuse. It occurs where an individual or group takes advantage of an imbalance of power to coerce, manipulate or deceive a child or young person under the age of 18 into sexual activity (a) in exchange for something the victim needs or wants, and/or (b) for the financial advantage or increased status of the perpetrator or facilitator. The victim may have been sexually exploited even if the sexual activity appears consensual. Child sexual exploitation does not always involve physical contact; it can also occur through the use of technology.’
Signs of CSE
Indicators that a child or young person may be being groomed may include:
- Being secretive about who they are talking to and where they are going;
- Often returning home late or staying out all night;
- Sudden changes in their appearance and wearing more revealing clothes;
- Becoming involved in drugs or alcohol, particularly if you suspect they are being supplied by older men or women;
- Becoming emotionally volatile (mood swings are common in all young people, but more severe changes could indicate that something is wrong);
- Using sexual language that you would not expect them to know;
- Premature sexual behaviour in under 16s;
- Engaging less with their usual friends;
- Appearing controlled by their phone; and
- Switching to a new screen when you come near the computer.
Indicators that an adolescent may be being exploited may include:
- Persistently going missing from school or home and/or being found out-of-area;
- Unexplained acquisition of money, clothes, or mobile phones;
- Excessive receipt of texts/ phone calls and/or having multiples handsets;
- Relationships with controlling/ older individuals or groups;
- Leaving home/ care without explanation;
- Suspicion of physical assault/ unexplained injuries including bruising;
- Suffering from sexually transmitted infections/ pregnancy;
- Parental concerns;
- Carrying weapons;
- Significant decline in school results/ performance;
- Gang association or isolation from peers or social networks;
- Becoming estranged from family;
- Self-harm or significant changes in emotional well-being; and
- Volatility in mood/ mood swings.
Types of Child Sexual Abuse +
Child sexual abuse covers a range of illegal sexual activities, divided into two categories – contact and non-contact abuse.
Contact abuse is where an abuser makes physical contact with a child, and it can include:
- Sexual touching of any part of a child, whether clothed or unclothed;
- Using a body part or object to rape or penetrate a child;
- Forcing a child to take part in sexual activities;
- Making a child undress or touch someone else.
Contact abuse can include touching, kissing and oral sex – sexual abuse is not just penetrative.
Non-contact abuse is where a child is abused without being touched by the abuser. This can be done in person or online and can include:
- Exposing or flashing;
- Showing pornography;
- Engaging in any kind of sexual activity in front of a child, including watching pornography;
- Making a child masturbate;
- Forcing a child to make, view or share child abuse images or videos;
- Forcing a child to take part in sexual activities or conversations online or through a smartphone;
- Possessing images of child pornography;
- Taking, downloading, viewing or distributing sexual images of children; and
- Not taking measures to protect a child from witnessing sexual activity or images.
Sexting
Children and young people who are involved in a sexting incident might have:
- Shared an image of themselves;
- Received an image from someone else;
- Shared an image of someone else more widely;
This may have happened with or without consent of all the people involved, and children may have been coerced or pressured into giving consent. It’s a criminal offence to create or share explicit images of a child, even if the person doing it is a child.
Signs of sexting
Sometimes a child might disclose that they have been involved in sexting, or they might mention something which gives cause for concern. Other times, professionals might notice that a child is behaving differently, being bullied, or overhear a conversation and the sexting might come to light when the professional tries to find out what is going on.
Poly-victimisation
Can be defined as the experience of multiple victimisations of different kinds – in different domains of a child’s environment – such as sexual abuse, physical abuse, bullying in school, witnessing community violence or being exposed to family violence. The emphasis here is on different kinds of victimisation, rather than multiple episodes of the same kind of victimisation. Research suggests that the greater number of victimisations experienced, the greater the impact on children’s mental health and wellbeing. When a child experiences any type of familial maltreatment, the risk for experiencing any other type of abuse or victimisation.
The concept of poly-victimisation raises the possibility of adopting a ‘contextual safeguarding approach’ in relation to intrafamilial child sexual abuse.
Referral of non-recent sexual abuse +
Sometimes an adult may disclose sexual abuse they suffered as a child (which can remain an ongoing traumatic experience), including within public, private, voluntary sectors and family settings. Responses to allegations by an adult of abuse experienced as a child must be at the same high standard of response to current abuse, because:
- There is a significant likelihood that a person who abused a child in the past will have continued and may still be doing so;
- Criminal prosecution may be possible if sufficient evidence can be carefully collated.
The adult who disclosed should be encouraged and supported to report the crime to the Police. If the adult will not report it to the Police, then the worker who the disclosure was made to must make a referral to the Police.
A referral should also be made to Children’s Services where the adult lived as a child and where the perpetrator lives now.
A referral to the Local Authority Designated Officer (LADO) should be made where the perpetrator works with children.
To make a referral to the LADO please email a LADO referral form to LewishamLADO@Lewisham.gov.uk
Emotional Support for Children and Young People +
Barnardos TIGER – Emotional Support Service
The Barnardos Tiger service offers emotional support for children and young people under 18 years old and up to 25 years old with Special Educational Needs where there has been a disclosure of sexual abuse or sexual assault or where the professional believes sexual abuse is likely.
What is TIGER?
- Short-term intervention; up to 15 sessions
- Evidence & trauma-informed approach
- Co-designed intervention plan, led by young person
- Using coaching to re-empower young person
Support offered in South East London:
- 1:1 meetings for young person
- 1-2 sessions of direct work with parent/carers
- Professional collaboration with team around the child
- Support onward referrals
- Training sessions for professionals
Useful information
T: 07519 294000
E: tigerservices@barnardos.org.uk
(Please note this is not a secure email address and should not be used for referrals)
To make a referral please visit: https://www.barnardos.org.uk/get-support/services/london-spa/tiger-referral
South London CSA Services
The South London CSA Services have produced a series of resources as part of NHS England’s ‘Enhancing sexual abuse pathway for CYP in South London’. These resources are available for all professionals working in the field of CSA within and outside of London.
The books are designed to help children (under 8 and 8-12 years old) and their families develop a shared understanding of what might happen after a child has been sexually abused.
Support for Practitioners +
The South London CSA Services have produced Best-Practice Guidance for Supporting Practitioners with Lived Experience of Sexual Harm. This guide is aimed at managers, practitioners and volunteers from therapy and support services, the voluntary sector, social care and related sector services.
Support for Non-Abusing Parents & their Family+
We Stand Charity
Visit their website: We Stand
We Stand offers a range of support services and information for families affected by Child Sexual Abuse.
The National Volunteer Helpline can be contacted on 0800 980 1958
Monday: 10am to 2pm
Tuesday: 10am to 2pm and 4pm to 6pm
Wednesday: 10am to 2pm
Thursday: 10am to 2pm
Email: support@westand.org.uk
Children & Adolescent Mental Health Services (CAMHS)
Lewisham CAMHS Introduction Video : CAMHS Offer Available to Lewisham Children and Young People
CAMHS Infrastructure
Lewisham Child and Adolescent Mental Health Services (CAMHS) offers therapeutic interventions to children and young people up to the age of 18 who experience mild to serious/complex mental health concerns that impact on daily living.
The service is made up of professionals from different backgrounds working together to provide multi-disciplinary care. This may include:
- Child and Adolescent Psychiatrists
- Clinical Psychologists
- Family Therapists
- Cognitive Behaviour Therapists
- Mental Health Nurses
- Occupational Therapists
- Psychotherapists
- Therapeutic Social Workers
- Child Wellbeing Practitioners
- Educational Well Being Practitioners
Lewisham CAMHS Services Summary and Contact Information
Services are provided at three key community sites within Lewisham Borough:
Kaleidoscope
32 Rushey Green, London, SE6 4JF
Tel: 020 3228 1000 or 020 3228 1001
Lewisham Park
78 Lewisham Park, London, SE13 6QJ
Tel: 020 3228 1001
Holbeach
9 Holbeach, London, SE6 4TW
Tel: 020 8314 9742
If you have any urgent concerns about a child or young person’s mental health or a referral query please contact the team at Kaleidoscope and ask to speak to a staff member on duty.
Tel: 020 3228 1000
Operating hours: Monday to Friday, 9am to 5pm (excluding bank holidays)
Emergencies out of hours: Please advise the parent, or carer to contact the child, or young person’s GP. In an emergency, if it is felt that the child or young person is not able to be kept safe, send them to their local A&E.
Crisis Support Line: South London and Maudsley NHS Foundation Trust operate a telephone support line that is available 24 hours a day if urgent help or advice is needed.
Tel: 0800 731 2864
Services at Kaleidoscope
Lewisham Generic Team (Horizon)
The Kaleidoscope Generic Team (Horizon) offers assessment, treatment and care for children and young people, up to the age of 18, who have significant emotional or mental health difficulties.
Crisis Service
The Child and Adolescent Crisis Service works with children and young people, up to the age of 18, who present at Lewisham University Hospital in crisis. The service also offers follow-up appointments in the community after discharge from hospital.
The Crisis Service also manages duty calls for urgent referrals, and in some cases can offer an appointment on the same day so that the child or young person does not need to attend A&E.
Child and Adolescent ADHD Team (Lewisham)
The Child and Adolescent ADHD Team provides treatment and care for children and young people with Attention Deficit/Hyperactivity Disorder (ADHD), up to the age of 18.
The team also provide guidance and consultation to professionals to discuss potential referrals and consultation to professionals who work with the young people in other settings such as schools.
Neuro-Developmental Team (NDT)
The Neuro-Developmental Team (NDT) offers assessment, treatment and care co-ordination for children and young people, up to the age of 18, with a significant learning disability and/or complex neurodevelopmental disorders.
The Lewisham CAMHS NDT supports children, young people, and their families, who may be experiencing anxieties around their health. The service is for children and young people who have had severe and complex problems for some time.
Child and Adolescent Paediatric Liaison Service
The Paediatric Hospital Liaison Service provides mental health input for children and young people children with acute illnesses, and those with chronic and life-limiting conditions.
The service co-ordinates psychological assessments for children and young people being cared for at University Hospital Lewisham. They can help manage the emotional impact of physical illness on children, young people and families, and improve their ability to manage the illness and its effects.
Child and Adolescent Schools Service (Lewisham)
The Child and Adolescent Schools Service (Lewisham) provides low-intensity, tier 2 assessment, treatment and care for children and young people, from 5 to 18 years old, who have mental health problems.
The service works mainly in Lewisham schools alongside education professionals; however, if necessary, they can offer home visits. Referrals are accepted from the Special Educational Needs and Disability (SEND) panel, New Woodlands School, the Outreach and Inclusion Service, and a small number of targeted schools.
Services at Lewisham Park
SYMBOL Team (Looked After Children)
The Symbol Therapy Team helps young people in local authority care in Lewisham who are struggling with mental health difficulties. The team also provide care for adopted young people living in Lewisham.
Symbol offer assessment, therapeutic intervention and care for young people, up to the age of 18, with moderate to severe emotional, behavioural and mental health problems. The team also offer a low-intensity service for young people leaving the care system, who are moving into adulthood.
The Lewisham Young People’s Service (LYPS)
The Lewisham Young People’s Service (LYPS) provide assessment and treatment for children and young people, up to the age of 18, who have ongoing severe and complex problems for some time that significantly affect their daily life.
LYPS also offers an early intervention service to young people who are experiencing psychosis.
Child and Adolescent Wellbeing Programme (Lewisham)
The Lewisham Children and Young People Wellbeing Practitioners (CWP) Team is a low-intensity, tier 2 service for children and young people who may not meet the threshold for mainstream CAMHS teams.
The CWP team provide short-term, low intensity, evidence-based, guided self-help interventions for children, young people and their parents. Treatment is available for mild to moderate anxiety, low mood, or mild behavioural difficulties.
Services at Holbeach
Adolescent Resource and Therapy Service (ARTS)
The Adolescent Resources and Therapy Service (ARTS) provide assessment, treatment and care for young people, up to the age of 18, who are known to a Youth Offending Service (YOS).
The ARTS team provide one to one and group treatment and care, and work with the police, the public protection unit, social services and our local Multi-Agency Public Protection Arrangement (MAPPA) team to support people in the community. The team also work with children and young people who exhibit sexually inappropriate behaviour.
Referrals
Please consult the CAMHS Referral Criteria for full information on services and referrals.
When making a referral to Lewisham CAMHS please use our CAMHS Referral Form
Non urgent referrals for CAMHS teams based at Kaleidoscope can be emailed to: LewishamCAMHSAdmin@slam.nhs.uk
Useful links
Young Minds - children’s mental health charity, which offers a host of advice and resources
Kooth - free online service that offers emotional and mental health support for children and young people
Samaritans - Charity aimed at providing emotional support to anyone in emotional distress
MindEd - free educational resource on children and young people’s mental health for adults
Royal College of Psychiatrists - Professional medical body responsible for supporting psychiatrists
Domestic Abuse & MARAC
Domestic abuse is defined as “any incident or pattern of incidents of controlling, coercive, threatening behaviour, violence or abuse between those aged 16 or over who are, or have been, intimate partners or family members regardless of gender or sexuality”. The abuse can encompass, but is not limited to:
- psychological
- physical
- sexual
- financial
- emotional
Domestic abuse can also include forced marriage and so-called “honour crimes”.
Controlling and coercive behaviour
Domestic abuse is often thought of as physical, such as hitting, slapping or beating, but it can also be controlling or coercive behaviour. This is important as what might look like an isolated incident of violent abuse could be taking place in a context of controlling or coercive behaviour.
Controlling behaviour is a range of acts designed to make a person subordinate and/or independent by isolating them from sources of support, exploiting their resources and capacities for personal gain, depriving them of the means needed for independence, resistance and escape and regulating their everyday behaviour.
Coercive behaviour is an act or a pattern of acts of assault, threats, humiliation and intimidation or other abuse that is used to harm, punish, or frighten their victim.
We know that the first incident reported to the police or other agencies is rarely the first incident to occur; often people have been subject to violence and abuse on multiple occasions before they seek help.
Learning resources to support health and social work in situations of coercive control
A set of learning resources for social workers, safeguarding leads, and health and social care practitioners, provides information and guidance on how to recognise and respond to coercive and controlling behaviour in intimate or family relationships.
Supporting the non-abusing parent in a holistic way that acknowledges the impacts of coercive control is important in achieving good outcomes for children. Research showed that children also experience the impacts of coercive control of a parent; for example, becoming isolated from family and friends, finding it difficult to gain independence, and feeling disempowered. The resources, which include five detailed case studies, will support practitioners to improve their understanding of the dynamics of power and control that underpin domestic abuse, enabling them to build trusting relationships with children and survivors.
The examples, tools and videos bring together evidence from research, practitioner experience, and the voice of people using services, to enable professionals to put the law into practice and improve support for people who are experiencing coercive control.
The Chief Social Worker’s Office at the Department of Health commissioned the materials, which were developed by Research in Practice for Adults and Women’s Aid. http://coercivecontrol.ripfa.org.uk/
Safeguarding children exposed to domestic abuse
Children who live in families where there is domestic abuse can suffer serious long-term emotional and psychological effects. Even if they are not physically harmed or do not witness acts of violence, they can pick up on the tensions and harmful interactions between adults. Children of any age are affected by domestic violence and abuse. At no age will they be unaffected by what is happening, even when they are in the womb.
The physical, psychological and emotional effects of domestic violence on children can be severe and long-lasting. Some children may become withdrawn and find it difficult to communicate. Others may act out the aggression they have witnessed, or blame themselves for the abuse. All children living with abuse are under stress.
Professionals should:
- Consider the presence of domestic abuse as an indicator of the need to assess a child’s need for support and protection
Safe Lives, a national domestic abuse charity, has created a toolkit practitioners and front-line workers can use to identify high risk cases of domestic abuse, stalking and ‘honour’-based violence. The purpose of the checklist is to give a consistent and simple-to-use tool to practitioners who work with victims of domestic abuse in order to help them identify those who are at high risk of harm and whose cases should be referred to a MARAC meeting in order to manage the risk.
The toolkit has been endorsed by agencies such as the police (Association of Chief Police Officers), National Centre for Domestic Violence, and CAFCASS, who believe that the primary audience should be front line practitioners working with victims of domestic abuse who are represented at MARAC. This will include both domestic abuse specialists such as IDVAs and generic practitioners such as those working in a primary care health service or housing.
Locally, both the Adult’s Safeguarding Board and Children’s Safeguarding Partnership (LSAB / LSCP), as well as the Safer Lewisham Partnership (SLP) have agreed that all agencies in Lewisham working with, or supporting families at risk of domestic violence are expected to use the risk checklist. This is vitally important because using an evidence based risk identification tool increases the likelihood of the victim being responded to appropriately and therefore, of addressing the risks they face. The risk checklist gives practitioners common criteria and a common language of risk.
Safe Lives have produced an updated version of the RIC, which now includes comprehensive guidance explaining each risk question, how they can be asked, as well as practice points. There is also a frequently asked questions page with some useful tips on the checklist. The Safe Lives website has helpful resources about other ways your agency may access support, training or download the checklist in other languages. The Lewisham Safeguarding Children’s Partnership also offers training on the use of the checklist which is free for all professionals in the borough to attend, however, for more questions about the use of the RIC, access to training, and questions about domestic violence MARAC process, please visit www.lewisham.gov.uk/vawg or contact the Violence Against Women & Girls (VAWG) Programme Manager on vawg@lewisham.gov.uk
Safeguarding high-risk victims of domestic violence and abuse – referring to the MARAC
The Lewisham Domestic Violence Multi-Agency Risk Assessment Conference (MARAC) is a risk management meeting where professionals share information on high and very high risk cases of domestic violence or abuse and put in place a risk management plan. The aim of the meeting is to address the safety of the victim, children and agency staff and to review and co-ordinate service provision in high risk domestic violence cases.
To be referred to the MARAC the individual must reside in the London Borough of Lewisham, be over the age of 16, be currently experiencing domestic violence or abuse (according to the cross Government definition of domestic violence)[1] and be assessed as being at high or very high risk of harm of domestic violence or abuse in accordance with the Lewisham MARAC referral risk criteria. In order to assess whether a case meets the risk threshold, the Safe Lives DASH MARAC risk indicator checklist should be completed by the referring agency.
A tailored action plan will be developed at the MARAC to reduce the risk to the victim, children, other vulnerable parties and any staff and to ensure that the risk the perpetrator presents is managed appropriately. Examples of actions that will be agreed include flagging and tagging of files, referral to other appropriate multi-agency meetings, prioritising of agencies’ resources to MARAC cases.
Any service agency signed up to the MARAC Information Sharing Protocol may refer a case to the MARAC using the Lewisham MARAC Referral Form, and all agencies should be actively screening for domestic violence or abuse. Referrals should be submitted to each agency’s MARAC representative. Please contact your line manager to find out who your agency’s MARAC representative is.
For more questions about the use of the MARAC, access to training, and questions about the process, please visit www.lewisham.gov.uk/vawg or contact the Violence Against Women & Girls (VAWG) Programme Manager on vawg@lewisham.gov.uk , or the MARAC Coordinator on dvmarac@lewisham.gov.uk
[1] https://www.gov.uk/guidance/domestic-violence-and-abuse
For further information
Letter to partners on the use of the DV risk assessment
visit www.saferlondon.co.uk/safer-lewisham
See the Domestic Violence information in our practice procedures
Useful Links:
Resources: http://imkaan.org.uk/resources
MOPAC VAWG Strategy 2018-2021
MOPAC Domestic and Sexual Violence Dashboard
Home Office Resources for Violence Against Women & Girls (VAWG)
Galop - The LGBT Anti-Violence Charity
Services Available to Lewisham Residents
Refuge, The Athena Service
The Athena service, run by Refuge provides confidential, non-judgmental support to those living in the London Borough of Lewisham who are experiencing gender-based violence. It opened its doors in April 2015 and provides outreach programmes, independent advocacy, group support, refuge accommodation and a specialist service for young women.
It provides the following services, all under one roof:
- One-to-one confidential, non-judgmental, independent support
- A specialist independent gender-based violence advocacy (IGVA) team to support clients at risk of serious harm
- A specialist service for 13-19 year-old girls
- Group support
- A peer support scheme to help break isolation; build social networks and provide support clients regain control of their lives
- Volunteering opportunities
Telephone: Athena Service on 0800 112 4052
Email: lewishamvawg@refuge.org.uk
Website: https://www.refuge.org.uk/our-work/our-services/one-stop-shop-services/athena/
African Advocacy Foundation
A community-led organisation working to promote better access to health, education and other opportunities for disadvantaged communities in the UK, Europe and parts of Africa.
African Advocacy provide practical support, policy work, advocacy, information, guidance and training to professionals and community members alike. African advocacy work to empower individuals and families experiencing multiple disadvantages and barriers including ill health, poverty, deprivation, violence, isolation and those relating to language, culture, faith and other social issues.
Location:
CATFORD (MAIN) OFFICES:
76 Elmer Road, Catford, London SE6 2ER
Telephone:
0208 698 4473
Website: https://www.africadvocacy.org/
BelEve UK
The purpose is to equip girls and young women with the right support, skills and confidence to make informed choices about their future; improve their educational, social and economic outcomes whilst taking control of their lives.
Location:
The Albany, Deptford, SE8 4AQ
Telephone:
0203 372 5779
Website: https://beleveuk.org/
Latin American Women’s Rights Service (LAWRS)
LAWRS has a zero tolerance policy of any form of Violence against Women and Girls (VAWG). Our team offers advice, advocacy and practical support to Latin American women who are experiencing or have experienced Domestic Violence, Harmful practices or any other form of violence.
Location:
Tindlemanor, 52-54 Featherstone Street.
London, EC1Y 8RT
Telephone:
020 7336 0888, 084 4264 0682
Website: http://www.lawrs.org.uk/
IKWRO – Women’s Rights Organisation
IKWRO are committed to providing non-judgmental support to women who speak Kurdish, Arabic, Turkish, Farsi, Dari, Pashtu and English.
Location:
IKWRO – Women’s Rights Organisation
PO Box 75229
LONDON
E15 9FX
Telephone:
0207 920 6460
Website: http://ikwro.org.uk/
Women and Girls Network (WGN)
WGN is a free, women-only service providing a holistic response to women and girls who have experienced, or are at risk of, gendered violence.
Telephone:
0808 801 0660
Website: http://www.wgn.org.uk/
WE Women (Women Empowering Women)
We Women is a collaboration of women which has been delivering community support to women since March 2017. In August 2018, we women became a constituted community group.
We Women are entirely volunteer run, and our aims are to:
- Empower women to be more self-sufficient
- Improve women’s health & well-being
- Address the material impacts of poverty within the local community
Location:
Pepys Resource Centre Old Library Deptford Strand London
London
Greater London
SE8 3BA
United Kingdom
Telephone:
020 8691 3146
Website: https://www.lewishamlocal.com/places/united-kingdom/greater-london/london/lewisham-groups/we-women-women-empowering-women/
Early Years Alliance - Lewisham Children's and Family Centres
The Alliance is working together with Clyde Nursery School, Beecroft Garden School and Kelvin Grove/Eliot Bank and Downderry Children’s Centres to deliver a clear seamless borough wide children’s centre offer for families in the London Borough of Lewisham, working alongside health visiting, midwifery, schools and public health services.
Lewisham Children and Family Centres offer families access to a range of health, education, play, parenting, adult education, employment support and family support services right across the borough.
Website: https://www.lewishamcfc.org.uk/
National Stalking Helpline – Suzy Lamplugh Trust
The National Stalking Helpline is run by Suzy Lamplugh Trust. Their mission is to reduce the risk of violence and aggression through campaigning, education and support.
Telephone: 0808 802 0300
Website: https://www.suzylamplugh.org/
METRO
METRO is a leading equality and diversity charity providing health, community and youth services across London and the south-east, with some national and international projects. METRO promotes health, wellbeing and equality through youth services, mental health services and sexual health and HIV services and works with anyone experiencing issues related to gender, sexuality, diversity or identity.
Location: 141 GREENWICH HIGH ROAD, GREENWICH, SE10 8JA
Telephone: 020 8305 5000
Website: https://metrocharity.org.uk/
RASASC - Rape & Sexual Abuse Support Centre Rape Crisis South London
RASAC believe too many women have had to be silent for too long about the violence perpetrated against them.
They understand that it can be difficult to speak up, hard to find the words or to believe that anyone will listen.
RASAC will listen. They believe. They will stand up alongside you. You do not have to do this alone.
Telephone: 0808 802 9999
Postal Address:
PO BOX 383, Croydon, CR9 2AW
Website: http://www.rasasc.org.uk/contact/
Stonewall
Information and campaigning for LGBT rights. Got a question? A problem? Need support? Stone wall are here to help with any issues affecting LGBT people or their families. Whatever your situation, you’re not on your own. Stonewall will do what they can to help or point you in the right direction to someone who can.
Telephone: 0800 0502020
Write to Stonewall: Stonewall 192 St. John Street London EC1V 4JY
Website: https://www.stonewall.org.uk/help-advice/contact-stonewalls-information-service
Respect
Men and women working together to end domestic violence
Telephone: 0808 802 4040
Address: The Green House
244-254 Cambridge Heath Road
London
E2 9DA
Website: http://respect.uk.net/
The Deaf Health Charity – Sign Health
www.signhealth.org.uk/our-projects/deafhope-projects/
Text: 07970350366
Rights of women
www.rightsofwomen.org.uk
Respect Helpline for men
0808 8010327
www.respectphoneline.org.uk/help-for-domestic-abuse-victims
Women's Aid live chat
This is an online chatting service which is ideal for victims who are self-isolating and do not want to be heard.
www.chat.womensaid.org.uk
www.womensaid.org.uk
0117 944 44 11
NSPCC Helpline - 0800 028 3550 or fgmhelp@nspcc.org.uk
GALOP National LGBT+ Domestic Abuse Helpline
0800 999 5428
www.galop.org.uk/domesticabuse
Difficult conversations with parents / carers
A guide for practitioners who work with children and their families.
The information in this guide is not exhaustive and it should be used as a reference alongside practitioners own safeguarding practices and in conjunction with appropriate supervision.
Four factors to consider when preparing for a difficult conversation with a parent or carer:
- Principles – that underpin safeguarding children.
- Planning – how to plan or be prepared
- The Conversation – things to consider when having a conversation
- Examples – open questions and suggestions
1. Principles – to support safeguarding discussions with parents / carers
- Always take time to plan the conversation before you speak to parents.
- Be open and honest, use basic language, avoid jargon.
- Ensure child protection policies are clear.
- Include child protection issues in information you give out to parents you are working with.
- Explain your statutory duty to safeguard children’s welfare, “duty of care” and requirement to report your concerns.
- Ensure parents / carers sign to acknowledge they have read and understood your safeguarding policy and offer them a copy.
- Use Early Help, refer to a children’s centre, or signpost to other support agencies, i.e. health visitor, parenting courses etc.
2. Planning
If you feel it’s too risky to talk to parents before speaking to Children’s Social Care, then don’t. Do not put yourself or a child at risk, e.g. if:-
- There is suspected sexual abuse.
- Parents could destroy evidence or hinder a police investigation.
- It is possible the child could be silenced.
Otherwise it’s good practice to discuss concerns with parents/carers and tell them you are going to make a referral. Before your conversation:-
- Plan how you are going to broach your concern and how to respond to different responses, e.g. anger, denial, emotional breakdown etc.
- Choose a time and place to give full privacy.
- Consider the timing of the meeting (e.g. a tired, crying baby, or collecting other children from school etc.) depending on the urgency of the concern.
- Adapt your style to the parent, consider language barriers or learning difficulties.
- Acknowledge your own anxiety about dealing with a difficult situation as it may affect your communication style.
- Have the child’s key worker with you or nearby for support and as a witness (and vice versa) or get support from Children’s Social Care.
- If previous experience of the parent/carer suggests they may pose a risk, make a full risk assessment and do not meet alone.
3. The Conversation
Make sure members of staff know where you are and what you are doing before a meeting. Tips and ideas for having a difficult conversation:-
- Consider your position in the room so nobody feels trapped.
- Ensure children cannot overhear you and are occupied (provide toys etc.)
- Frame the concern in a model of help and support.
- Be straight forward – Tell the parent/carer a referral to the Multi-Agency Safeguarding Hub is going to be or has been made.
- Tell them that “as a parent/carer they will want to get to the bottom of the matter”.
- Give clear explanations.
- Always remain confidential and professional.
- Words are sometimes really hard to find when approaching a parent – use ‘active listening’.
- Do not argue, interrupt, give advice, pass judgement, jump to conclusions or let the parent’s sentiment affect you.
- Avoid excessive reassurance, it may not be all right.
- Do encourage the parent to talk.
- Clarify what the parent means.
- Summarise what the parent has said.
- Consider your communication style: tone, pitch, speed of voice, body language (body slightly to the side, with an open stance or sit) be clam, make eye contact and appreciate they may need to talk.
- Consider the parents point of view which may be influenced by; bad experience of services, lack of trust, limited or distorted understanding of what is appropriate for children, learning difficulties, cultural and language barriers.
- Explain the nature of your concern using tact and diplomacy, but be direct and use factual information “Jodie was not brought to the last 2 appointments, what is the reason for this?”
- Do not use words such as child protection or child abuse, try words such as concerns, welfare, and duty of care.
Use your eyes and ears more than your mouth.
4. Examples
This is not an exhaustive list and you may want to use a technique of your own, following the general principle of open and probing questions:
- Avoid using “I think” which indicates it could be your own opinion.
- Avoid using jargon, try:-
- “I need to talk to you about the injury to XY’s face, can you tell me what happened?”
- “XY has been very lethargic today and says he has not slept, is there anything going on that might be troubling him?”
- “XY’s behaviour has changed dramatically over the last few weeks, (s)he has gone from being a happy, outgoing child to a very quiet, withdrawn child. Have you any idea what could have caused this?”
- “Whenever there is a worry about any child, or they something about being hurt we legally have to pass on that information to children’s services – you may have read this in the parent’s information/handbook when XY started?”
- “XY told a member of staff he is slapped every night, and, because of what he has said I have informed Children’s Social Care. All settings are expected to talk to Children’s Social Care when children say things like this, and Children’s Social Care have asked me to talk to you about this. Can you tell me what happened?”
Questions can start with the following:-
- “is there any reason why……….”
- “we need to have a chat………..”
- “XY has said……………………..”
- “I have noticed XY has seemed hungry in the mornings, is (s)he managing to have breakfast before he comes to school?”
- XY has a bruise on his face but he can’t remember how it happened, do you know how he did it?”
Next steps?
Once you have had a conversation or a series of discussions with the parent or carer, you may need to consider what actions, if any, you need to take. Consider the following:-
- Professional curiosity – have you confirmed the response you have received from other agencies? Do you need to make further enquiries?
- Trust your instincts – You have spoken to the parent/carer and you know the child – trust your instincts if you still have concerns.
- Follow safeguarding procedures – ensure you check your agency safeguarding procedures and seek guidance from an appropriate person.
- Pre and Post Supervision – agencies have varying supervision procedures; be sure to raise your concerns and get guidance and support before and after you have had a conversation with a parent/carer as this will give you a chance to reflect on what happened and discuss what needs to happen next (reflective practice).
- Escalation – If you are still concerned about a decision or practice you can escalate your concerns; the LSCP recommend you follow our Resolving Professional Differences / Escalation Policy.
- Referral – Following any discussion, if you are concerned about the safety of a child or you believe they are at risk of immediate danger – contact the police. If you believe the child is at risk of significant harm – seek guidance from the MASH team.
- Early Help – You may want to contact Early Help or create a Team Around the Family.
| What are we worried about? |
What’s working well? |
What needs to happen? |
|
What words would you use to talk about this problem so that parents/carers understand?
Use plain language and avoid jargon.
Consider any problems the family might be having which are making this problem harder to deal with e.g. housing, finances, isolation, or family breakdown.
Example questions:-
- I need to talk to you about the mark XY’s face, (s)he can’t remember how it happened, and do you know how (s)he did this?
- XY’s behaviour has changed a lot in the last few weeks. (S)he has gone from being happy and outgoing to quiet and withdrawn – have you any idea what might have caused this this?
- We are having a lot of problems with XY, (s)he seems angry. Is there anything happening at home which would help us to understand this?
- I know we have talked about this before but I am still worried because XY is still quite dirty when she comes to school and other children have commented that (s)he smells. Do you have everything you need at home to wash clothes and to have a bath regularly?
|
Who are the people who care for the child? And what are the best things about how they care for them?
Who would the child say are the most important people in their lives? And how do they help them grow up well?
Example questions:-
- It sounds like things are a bit difficult at the moment, is anyone supporting you?
- What would XY say are the best things about his life?
- You have been doing well to get XY to school with all that is happening, is there anything we can do to support you further?
- Have you noticed this problem before? How was it sorted out in the past?
|
Now you have explored this more, how worried are you about this child? 10 is not worried; 0 is so worried you need to make a referral for support or safeguarding.
- What would you need to see for it to be 10?
- What do you think is the next step to getting this worry sorted out?
- Have you done any direct work with the child?
Next steps:
- Curiosity – verify any information with professionals or other family members.
- Supervision – seek guidance before and after interaction with parents/carers to reflect on the information gathered.
- Procedures – follow your agency safeguarding procedures.
- Referral – If you are concerned about the safety of the child or young person.
- Escalation – If you are not satisfied with the outcome of the referral and still have concerns.
|
Discharge & Safety Planning Protocol for Lewisham Children & Young People
For Children and Young People who present and require a multi-agency response to address
their safeguarding and mental health needs)
July 2022
Partners to the Protocol
- Lewisham and Greenwich NHS Trust
- London Borough Lewisham, Lewisham Children’s Social Care
- South London and Maudsley NHS Foundation Trus
Purpose and Scope
The purpose of this protocol is to support multi-agency practitioners to make appropriate arrangements which support the safe and timely discharge of children and young people under 18 years of age.
The protocol is intended to ensure that all practitioners are clear about the steps to take to ensure that no child is discharged from hospital into an unsafe environment, where their health or well-being may be compromised or where further significant harm could occur.
The protocol applies to children and young people who require a multi-agency response to address their needs. A multi-agency response may be required due to:
- Serious or complex mental health needs requiring hospital admission;
- Self-harm or attempted suicide; or have expressed an intention to do either;
- Safeguarding and other welfare concerns cover situations where there is known or suspected neglect or abuse;
- Exploitation or neglect is known prior to admission, and this is recent or current, it would be expected that these children have an allocated social worker);
- The child/young person is looked after;
- Abuse, exploitation or neglect comes to light or is suspected during the hospital admission, Children subjected to Trafficking/FGM/ Modern Slavery;
- Ward Staff raise concerns about the parent/child interaction, Parent/Carer whose understanding or concern for their child is lacking. Children or young people in Police custody or due to be arrested upon discharge.
- Children or young people who have been the victim of physical or sexual assault;
- The Child/Young Person says they do not want to return home;
- This is not an exhaustive list and professionals should apply their professional judgement and consult with their named safeguarding leads if they have any concerns at all about a child/young person.
Principles
Any child or young person, who self-harms or expresses thoughts of self-harm or suicide, must be taken seriously and appropriate help and intervention, should be offered at the earliest point. Any practitioner, who is made aware that a child or young person has self-harmed, or is contemplating this or suicide, should talk with the child or young person without delay.
Most children who have been admitted with mental health needs will need on-going community care for a period of time after discharge. Follow up services for the young person’s mental health services could include, outreach sessions, liaison with local services, and outpatient therapy sessions and will be determined by the local CAMHS service following assessment.
Discharge planning is an essential part of care management in any hospital setting. It ensures that health and social care systems are proactive in supporting individuals and their families in the community. It needs to start early to anticipate problems, put appropriate support in place and agree service provision. Consideration should be given to the wider environment the child will be returning to, including siblings and other members of the household.
Children should not remain in hospital once they are well enough to leave. However, it is essential that when a child is in hospital and there are safeguarding concerns about the child, effective multi-agency planning between key professionals working with the child is undertaken before the child is discharged from hospital. Where there are safeguarding concerns, a referral must be made to Lewisham Children’s Social Care.
All agencies have a duty to share information and a joint responsibility to work together to protect children and promote their wellbeing and safety. Referrals to Lewisham Children’s Social Care must be made to MASH service who will determine the level of response by processing information through the multi-agency safeguarding hub.
Linked Policies and Procedures
The protocol should be read in conjunction with:
- The London Child Protection Procedures
- LGT Safeguarding Guideline for Paediatricians Algorithm for Safeguarding
- LGT Safeguarding Children & Young People Policy
The Full Protocol Content
Lewisham Discharge Protocol for Children and Young People - July 2022
Emotional Abuse of Children & Young People
Working Together 2018 Definition
The persistent emotional maltreatment of a child such as to cause severe and persistent adverse effects on the child’s emotional development.
It may involve, include, or be conveyed to a child:-
- They are worthless or unloved.
- Inadequate.
- Valued only insofar as they meet the needs of another person.
- Not giving the child opportunities to express their views, deliberately silencing them or “making fun” of what they say or how they communicate.
- Age or developmentally inappropriate expectations being imposed on children. These may include interactions that are beyond a child's development capability, as well as an overprotection and limitation of exploration and learning, or preventing the child participating in normal social interaction.
- Seeing or hearing the ill-treatment of another.
- Serious bullying (including cyber bullying),
- Causing children frequently to feel frightened or in danger
- Exploitation or corruption of children.
Other forms of emotional abuse may be:-
- Ignoring, e.g. withdrawal of attention or rejection.
- Belittling, e.g. telling the child he or she is 'no good', 'worthless', 'bad', or 'a mistake'.
- Shamming, humiliating or name-calling
- Using extreme forms of punishment, such as confinement to a closet or dark room, tying to a chair for long periods of time etc.
- Emotional abuse is the 2nd most common reason for children needing protection from abuse in the UK.
- Some level of emotional abuse is involved in all types of maltreatment of a child, though it may not occur alone.
Passive Emotional Abuse
NSPCC. When a parent / carer denies their child the love and care they need in order to be healthy and happy. It’s known as passive abuse.
Five categories of passive emotional abuse have been identified (Barlow and Shrader McMillan 2010).
- Emotional unavailability
where a parent or carer is not connected with the child and cannot give them the love that they deserve and need.
- Negative attitudes
such as having a low opinion of the child and not offering any praise or encouragement.
- Developmentally inappropriate interaction with the child
either expecting the child to perform tasks that they are not emotionally mature enough to do or speaking and acting in an inappropriate way in front of a child.
- Failure to recognise a child’s individuality
this can mean an adult relying on a child to fulfil their emotional needs and not recognising that the child has needs.
- Failure to promote social adaptation
not encouraging a child to make friends and mix among their own social peers.
Why Might Emotional Abuse Happen?
Periods of high stress and tension, such as money worries or unemployment, can take a parent(s)/carer(s) focus away from providing the emotional support that a child needs. Additionally to the above they may be emotionally unavailable, because they’re not around or too tired. Forget to offer praise or encouragement. Expect a child to take on too much responsibility for their age, for example caring for other family members (refer to Lewisham Young Carers). If a parent had a bad experience when they was a child or has bad role models around them now, then this can affect how they look after their own children.
Short & Long Term Effects of Emotional Abuse
A child experiencing emotional abuse may develop social withdrawal, aggressive behaviour, may appear withdrawn may regress in their behaviour, develop sleep disorders, have nightmares, and self-harm. If unresolved these conditions can continue into adulthood and lead to more maltreatment, eating disorders, mental health issues and substance misuse disorders.
Action to take
- Be alert to the signs of emotional abuse.
- Try to speak to the child or young person alone to seek further information and clarification about what they are experiencing and how they are feeling.
- If the child or young person reports they are being emotionally abused you should listen to them, take their allegations seriously, and reassure them you will take action, including what the actions will be. If the child is worried about any of your actions, including speaking to the parent / carer, explain why and how you are going to help make it better for them and discuss their concerns to reassure them.
- If you are not the Designated Safeguarding Lead (DSL), report your concerns to your appointed DSL. If you are the DSL you should talk to the parent / carer and explain the concerns raised and inform them of the action you are going to take, i.e. make a referral to the MASH Team.
Make a Referral to MASH
If a child is in immediate risk call 999, otherwise contact the MASH Team by telephone and follow up your referral in writing within 24 hours.
MASH Team Telephone: 020 8314 6660
Email mashagency@lewisham.gov.uk
NSPCC & ChildLine
The NSPCC have had a 200% increase in 7 years in reports of emotional abuse, receiving 27 calls a day on average from children and young people.
It is important that children and young people feel safe and know who they can talk to when they are experiencing any kind of abuse.
ChildLine Number 0800 1111
Website: www.childline.org.uk
How Safe Are Our Children? NSPCC Annual Report
The NSPCC have completed the most comprehensive overview of Child Protection in the UK in 2018 in their annual report. It compiles and analysis data from the across the UK to show the current child protection landscape.
Key Findings:-
- An increase in police-recorded child sexual offences across the UK.
- Increases in child cruelty and neglect offences in all UK nations except Scotland.
- Increased numbers of children on child protection plans and registers over the last decade.
To read the full report click here NSPCC How Safe Are Our Children 2018
Guidance & Resources
Escalation Policy - Resolving Professional Differences
Having different professional perspectives within safeguarding practice is a sign of a healthy and well-functioning partnership. These differences of opinion are usually resolved by discussion and negotiation between the professionals concerned. It is essential that where differences of opinion arise they do not adversely affect the outcomes for children and young people, and are resolved in a constructive and timely manner.
Differences could arise in a number of areas of multi-agency working as well as within single agency working. Differences are most likely to arise in relation to;
- Criteria for referrals
- Outcomes of assessments
- Roles and responsibilities of workers
- Service provision
- Timeliness of interventions
- Information sharing and communication
If you have difference of opinion with another professional, remember:
- Professional differences and disagreements can help us find better ways improve outcomes for children and young people
- All professionals are responsible for their own cases, and their actions in relation to case work
- Differences and disagreements should be resolved as simply and quickly as possible, in the first instance by individual practitioners and /or their line managers
- All practitioners should respect the views of others whatever the level of experience. Remember that challenging more senior or experienced practitioners can be hard
- Expect to be challenged; working together effectively depends on an open approach and honest relationships between agencies
- Professional differences are reduced by clarity about roles and responsibilities and the ability to discuss and share problems in networking forums
Where immediate resolution cannot be found, professionals should make accurate records of discussions and correspondence and follow the LSCP Inter-Agency Escalation Policy. When making a referral to the LSCP please email safeguardingpartnership@lewisham.gov.uk.
Fabricated or Induced Illness and Perplexing Presentations Guidance
MULTI-AGENCY GUIDANCE FOR THE MANAGEMENT OF
PERPLEXING PRESENTATIONS, OR, SUSPECTED FABRICATED OR INDUCED ILLNESS
1. Introduction
This guidance is written to support multi-agency frontline practitioners to make appropriate decisions on how to safeguard children who present with perplexing presentations (PP) and Fabricated or Induced Illness (FII), additionally advise practitioners on how to recognise these issues, how to assess risk and how to manage these types of presentations in order to obtain better outcomes for children.
This guidance is based on the Royal College of Paediatrics and Child Health (RCPCH) 2021 guidance Perplexing Presentations (PP)/Fabricated or Induced Illness (FII) in children – guidance – RCPCH Child Protection Portal as well as learning from Serious Case Reviews, and aims to put the RCPCH 2021 document in context for practitioners working in Lewisham.
Whilst mainly applicable to health practitioners, this multiagency guidance is applicable to all frontline staff working with children, young people, and their families.
The term ‘children' or ‘child’ applies to all children and young people who have not yet reached their 18th birthday as per the Children Act 1989. The fact that a child has reached 16 years of age; is living independently or is in further education; is a member of the armed forces; is in hospital; in prison or in a young offender's institution, does not change his or her status or entitlement to services or protection under the Children Act 1989.
2. Purpose
The purpose of this policy is to:
- Provide Lewisham frontline practitioners with a single consistent approach in the management of PP, or suspected FII.
- Advise safeguarding partnerships of a single consistent approach across local providers and staff in the management of PP, or suspected FII.
- Provide staff with the information and guidance they need to fulfill their statutory duties to safeguard and protect children and young people when there is suspected PP or FII.
- Clearly define roles and responsibilities so that the process is transparent, and staff understand the complexities involved and have realistic expectations about the timeframes within which any given case can be managed.
LSCP Multi-agency Guidance for the management of Perplexing Presentations, or, suspected Fabricated or Induced Illness
Appendix 1 : Generic flow chart when there are alerting signs
Appendix 2 : Spectrum of cases where FII concerns may arise (RCPH, 2013)
Appendix 3 : Sample of chronology template
Appendix 4 : Health and education rehabilitation plan template
Tri-Borough 7 Minute Briefing : Fabricated & Induced Illness and Perplexing Presentations
14. References
Female Genital Mutilation / Cutting
Between April 2022 and June 2022 there were 745 newly recorded women and girls presenting at
Health settings in London,where FGM was identified or a procedure of FGM was undertaken.
NHS Digital FGM Annual Report April 2022-June 2022
What is FGM?
FGM is a form of violence against women and girls (VAWG). It comprises of all procedures involving partial or total removal of the external female genitalia for non-medical reasons. It may be carried out at any time in a girls life, from baby to womanhood. It can be seen as a pathway to womanhood and can also be a condition of marriage. Some communities believe that if a girl has not had it done she is deemed unhealthy, unclean, or unworthy. Parents can have very strong beliefs, genuinely thinking they are doing the right thing for their daughter, and in communities where all females have the procedure it can seem normal, then making it very difficult for girls to challenge this tradition. However, not every mother who has had FGM will put their daughter(s) through the same procedure. Each case should be assessed carefully and sensitively.
It is sometimes also known as female circumcision. Other local terms are: Tahoor, Absum, Halalays, Khitan, Ibi, Sunna, Gudnii, Bondo, Kutairi. It is important to let the female refer to the term she understands it to be called. FGM is sometimes incorrectly believed to be an Islamic practice. This is not the case and the Islamic Shari’a Council, the Muslim College and the Muslim Council of Britain (MCB) have condemned the practice of FGM. The majority of cases of FGM are thought to take place between the ages of 5 and 8 and therefore girls within that age bracket are at a higher risk.
Mandatory Reporting Duty - What are ‘known cases?
Known cases are those where either a girl informs the person that an act of FGM – however described – has been carried out on her, or where the person observes physical signs on a girl appearing to show that an act of FGM has been carried out and the person has no reason to believe that the act was, or was part of, a surgical operation within section 1(2)(a) or (b) of the FGM Act 2003. The duty applies to all regulated professionals working within health or social care, and teachers. There is mandatory requirement to report to police cases of ‘visually identified’ or ‘verbally disclosed’ cases of FGM in girls under 18. The mandatory reporting does not apply to suspected cases or where a child might be ‘at risk’ of FGM. The mandatory reporting is for ‘known’ cases only.
It is Illegal
In the UK, anyone found guilty of an FGM offence or of helping somebody commit one, faces up to 14 years in prison, a fine, or both, regardless of where in the world the FGM takes place. Anyone found guilty of failing to protect a girl from risk of FGM faces up to 7 years in prison, a fine, or both. Lewisham has secured 1 FGM Protection Order.
Recognising Signs & Symptoms of Possible FGM Cases
A girl may;
- Say an older female relative is coming especially to see her.
- Say that she is being taken "home" for a special visit to become a woman (right of passage).
- become withdrawn following this "holiday" and/or there may be a change in her behavior.
- Run away from home, or start truanting from school.
- Have difficulty standing or sitting.
- Spend longer in the toilet than usual; because of bleeding and/or infection.
- Have frequent vaginal, urinal, or pelvic infections.
- Blood born infections, including Hepatitis B & C, and HIV.
- She may be reluctant to undergo any medical examinations.
- May ask for help, but not be explicit about the problem due to fear or embarrassment
- Develop emotional and mental health problems.
- Self harm, or be showing signs of child abuse.
Long Term Health Effects
Many girls and women are not aware of the lifetime effects FGM can have on them; with difficulty in child birth (sometimes ending in death), infertility, sexually difficulties, vaginal infections, painful periods, cysts and abscesses, and difficulty controlling her bladder. This is a procedure that cannot be reversed. FGM also involves a long term emotional impact including, anxiety, depression, and post traumatic stress disorder.
FGM is classified into four categories:
- Clitoridectomy: partial or total removal of the clitoris and, in very rare cases, only the prepuce
- Excision: partial or total removal of the clitoris and the labia minora, with or without excision of the labia majora
- Infibulation: narrowing of the vaginal opening through the creation of a covering seal. The seal is formed by cutting and repositioning the inner, or outer, labia, with or without removal of the clitoris
- Other: all other harmful procedures to the female genitalia for non-medical purposes, e.g. pricking, piercing, incising, scraping and cauterizing the genital area
Language & Image Guide - Please refer to the current language and image guidance to use when talking to survivors of FGM.
The following are terms used by different nationality's to describe FGM. You will need to consider that a survivor may not recognise FGM or Cutting to describe what they have experienced.
- Egypt: Thara / Khitan / Khifad
- Ethopia: Megrez / Absum
- Eritrea: Mekhnishab
- Kenya: Kutairi / Kutairi was ichana
- Nigeria: Ibi / Ugwu / Sumna
- Sierra Leone: Sunna / Bondo / Bondo Sonde
- Somalia: Gudiniin / Halalays / Qodiin
- Sudan: Khifad / Tahoor
- CHAD: Bagtne / Gadja
- Guinea-Bissau: Fanadu di Mindjer / Fanadu di Omi
- Gambia: Niaka / Kuyango / Musolula Karoola
Procedure in Lewisham
The LSCP Partnership has endorsed a local FGM Guidance to assist you with your responsibilities.
At-Risk Cases of FGM
Situations whereby the female child is at risk of FGM being performed, suspected of being performed, or suspected of having been performed, normal safeguarding procedures and existing pathways would apply. You should consult with your appointed safeguarding lead and you should report it to MASH on 020 8314 6660 and email mashagency@lewisham.gov.uk.
An FGM Protection Order offer a legal means to protect and safeguard victims and potential victims of FGM. Please see the Fact Sheet for more information.
Reporting Known Cases in Lewisham
In London the only reporting gateway for mandatory reports is via 101. You should also inform MASH and your appointed safeguarding lead of your report.
The duty applies to all regulated professionals working within health or social care, and teachers. There is mandatory requirement to report to police cases of ‘visually identified’ or ‘verbally disclosed’ cases of FGM in girls under 18. The mandatory reporting does not apply to suspected cases, or where another person (including the mother) discloses that FGM has taken place, or where a child might be ‘at risk’ of FGM. The mandatory reporting is for ‘known’ cases only, and this can be any girl of any nationality.
Home Office Mandatory Reporting Procedural Guidance
Government Safeguarding women and girls at risk of FGM: FGM Safeguarding Pathway, Quick Guide for Health Professionals and templates.
Multi-Agency Statutory Guidance FGM
Support is Available for Girls and Women at Risk
You can obtain a Statement Opposing Female Genital Mutilation for girls and women. It is in a variety of languages on the GOV.UK website. Girls and Women can also contact;
- Athena VAWG Service on 0800 112 4052, email lewishamvawg@refuge.org.uk, website www.refuge.org.uk/Athena
- African Advocacy Foundation on 020 8698 447, website http://www.africadvocacy.org/
- NSPCC FGM Helpline on 0800 028 3550, email fgmhelp@nspcc.org.uk
- FGM Every Bodys Biz website provides advice, support and a forum to hear the voice of the girl/woman. You can also obtain up-to-date information on FGM Health Specialists and organisations working on FGM, http://fgm-every-bodys-biz.co.uk/
- If a girl or woman has been taken abroad phone the Foreign & Commonwealth Office immediately on 020 7008 1500.
Specialist FGM Clinics for Survivors of FGM
African Well Women’s Clinic
Guy’s & St Thomas’ Hospital, 8th Floor, c/o Antenatal Clinic, Lambeth Palace Road, London SE1 7EH
Tel: 020 7188 6872
Open Monday-Friday, 9am to 4pm.
Contact: Confort Momoh MBE, FGM / Public Health Specialist 07956 542 576
Action African Well Women Centre
Self Referral for free confidential services
Contact: Julia Albert – Midwife or Hayat Arteh – Health Advocate
Tel: 020 8383 8761 or 07956 001 065
or 07730 970 738
Manor Gardens Clinic
The project works with volunteer FGM Community Champions, delivers training, provide workshops and 1:2:1 support through the Dahlia project (Specialist therapeutic service for women who have undergone FGM).
E-Learning
For further information on FGM we would encourage all professionals to view the excellent Home Office training package on FGM which can be found at: www.fgmelearning.co.uk/
Useful Links & Guidance:
NHS England Posters & Guidance
National FGM Centre
FGM Map by Country & Origin and their Practice
FGM Health Passport- Statement opposing FGM guidance in different languages.
Links to information about FGM Orders:-
National FGM Centre
Courts of Justice - Family Procedure Rules
What to do if you are worried about the Safety of a child – professionals
Female Genital Mutilation - An Overview (leaflet)
Forced Marriage - Right to Choose
This document sets out the duties and responsibilities of agencies with the aim of protecting children and adults facing forced marriage. It does not attempt to replicate existing safeguarding guidance but should form part of all the existing child and adult protection structures, policies and procedures.
The document highlights specific arrangements that may inadvertently place a victim at risk of harm. These include failure to share information appropriately between agencies, the involvement of families, breaches of confidentiality and all forms of family counselling, mediation, arbitration and reconciliation.
Full Guidance: The right to choose: government guidance on forced marriage - GOV.UK (www.gov.uk)
Free E-Learning: Awareness of Forced Marriage
Learning outcomes:
- Recognise the warning signs of forced marriage.
- Take the right actions to help protect the potential victim.
- Cooperate effectively with other agencies.
Harmful Sexual Behaviour
Lewisham CAMHS ARTS Team HSB/AIMS Flow Chart
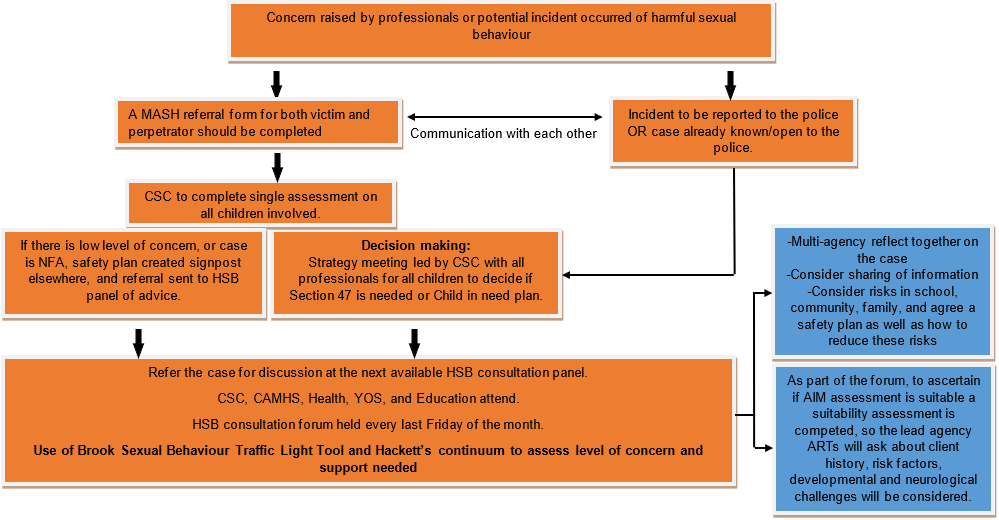
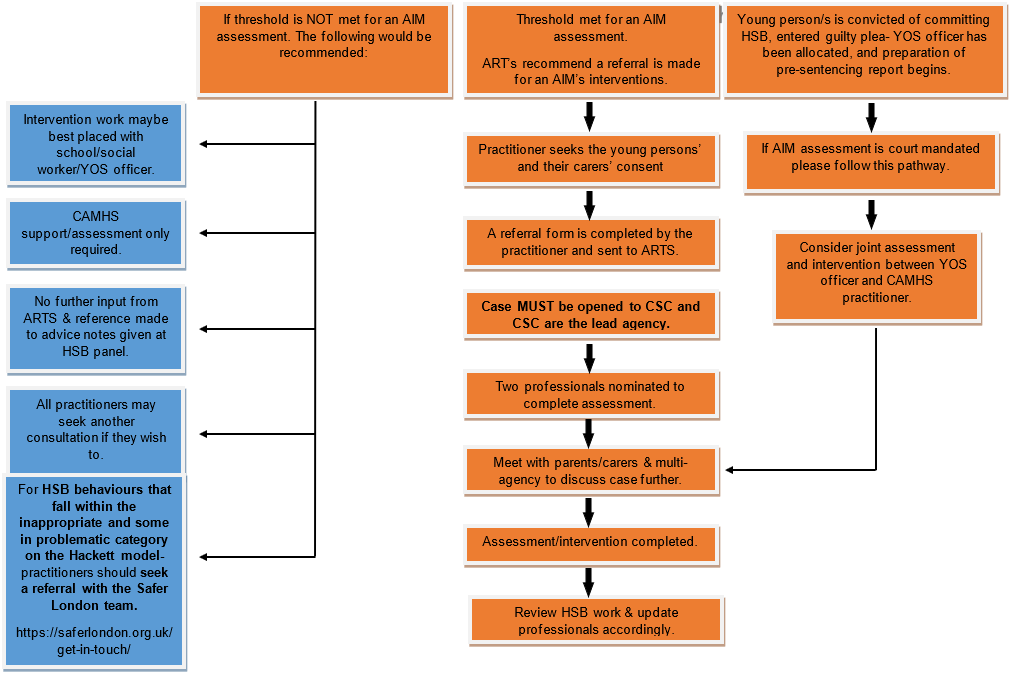
HSB: Harmful Sexual Behaviour; CSC: Children's Social Care; NFA: No Further Action, MASH: Multi-Agency Safeguarding Hub; AIM: Assessment Intervention & Moving on; YOS: Youth Offending Service; CAMHS: Child & Adolescent Mental Health Service.
NEW HARMFUL SEXUAL BEHAVIOUR PATHWAY / MONTHLY CONSULATION PANEL IN THE LONDON BOROUGH OF LEWISHAM +
ARTS (Adolescent Resource Therapy) TEAM +
Who are the ARTS team?
The service aims are to:
- Assess and treat the mental health needs of young people in the criminal justice system (CJS) and those whose offending behaviour could lead them into the criminal justice system.
- Work with young people involved in the CJS or Children’s Social Care (Lewisham) showing signs of sexually inappropriate behaviour.
- Ensure through integrated working that all YOS interventions are trauma informed.
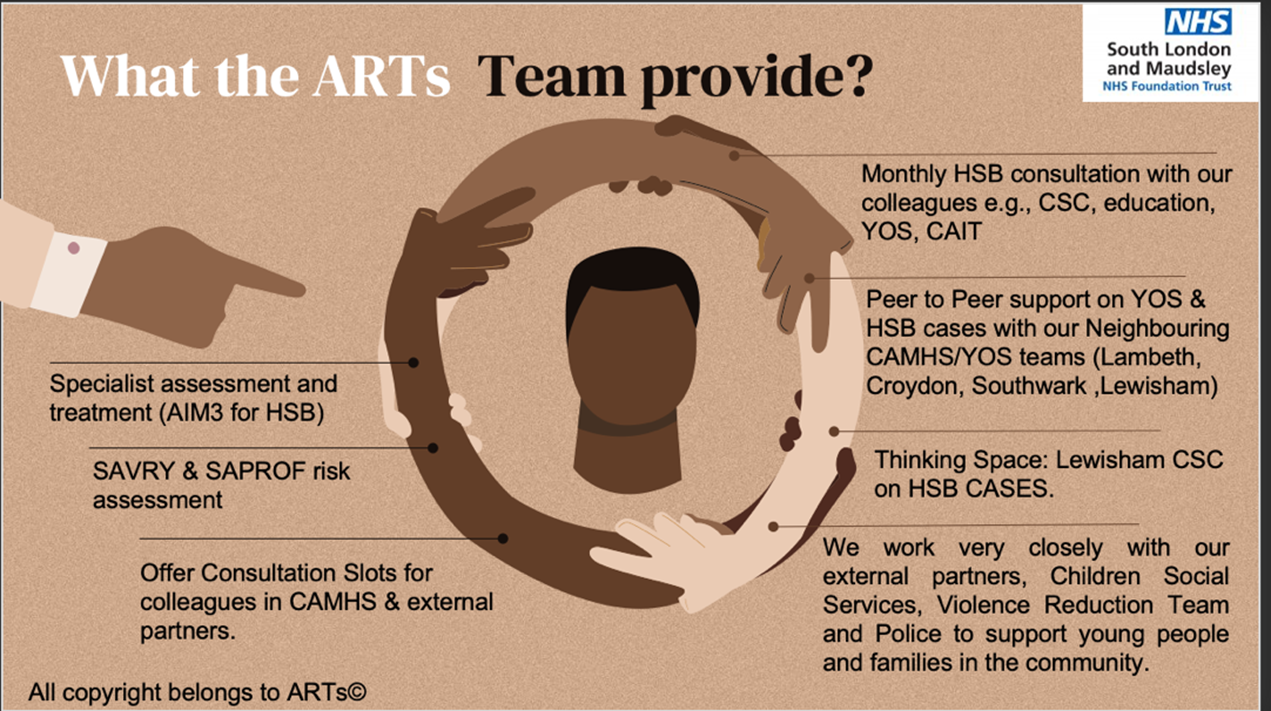
What is Harmful Sexual Behaviour (HSB)? +
Children and adolescents display a range of different sexualised behaviours. However harmful sexual behaviour (HSB) is developmentally inappropriate sexual behaviour displayed by young adults and adolescents, which may be violent and abusive (Hackett, 2014). To help professionals working with young people to distinguish between developmentally typical sexual behaviours from sexual behaviours that are problematic, and how to respond, the Hackett’s Model of HSB is a helpful tool to use (shown below)

Here is a video by NSPCC learning on why HSB’s a safeguarding concern and child protection concern: https://www.youtube.com/watch?v=hnLQFUi6uWk
Many young people referred into mental health services for HSB have experienced abuse, trauma (Hackett et al., 2013), and have several other psychosocial complex needs. Young people who display HSB may also develop further behavioural problems, for instance, poor self-regulation/coping skills, post- traumatic stress disorder (PTSD), depression, anxiety disorders, poor attachments and self-esteem, deficits in social skills, and have poorly defined personal boundaries sometimes on the background of neurodevelopmental difficulties (Hollis, 2017; Rich, 2011). Given the complexity of these cases a thinking space should be provided to consider risk factors in order to appropriately target the intervention and prevent future occurrences.
Further to this, the NICE guidelines explicitly state as part of their recommendations that “children’s social care services should identify services employing staff with the skills to undertake a specialist assessment of risk for children and young people displaying HSB” this includes child health services such as CAMHS.
The forum aims to:
- Have multi-agency representation when considering harmful sexual behaviour (HSB) cases.
- Act as a steering group.
- Act as the referral route for Lewisham CAMHS Forensic Team.
- Act as a source of knowledge, expertise and support for the practitioner presenting the case at the forum.
**For any HSB behaviours that fall within the inappropriate category on the Hackett’s model, practitioners and clinicians should seek a referral with the Safer London Team**
Aims & Objectives of the Monthly Consultation Panel +
In the borough of Lewisham, multi-agencies aim to work together to provide a specialist service to children and young people who have engaged in harmful sexual behaviour (HSB). This includes harm to other children, young people, and themselves.
**Please note this consultation space will not be attempting to formulate the HSB behaviour but provide a reflective space to all presenting practitioners, and give consideration to the safety planning and risk management **
Purpose of the panel +
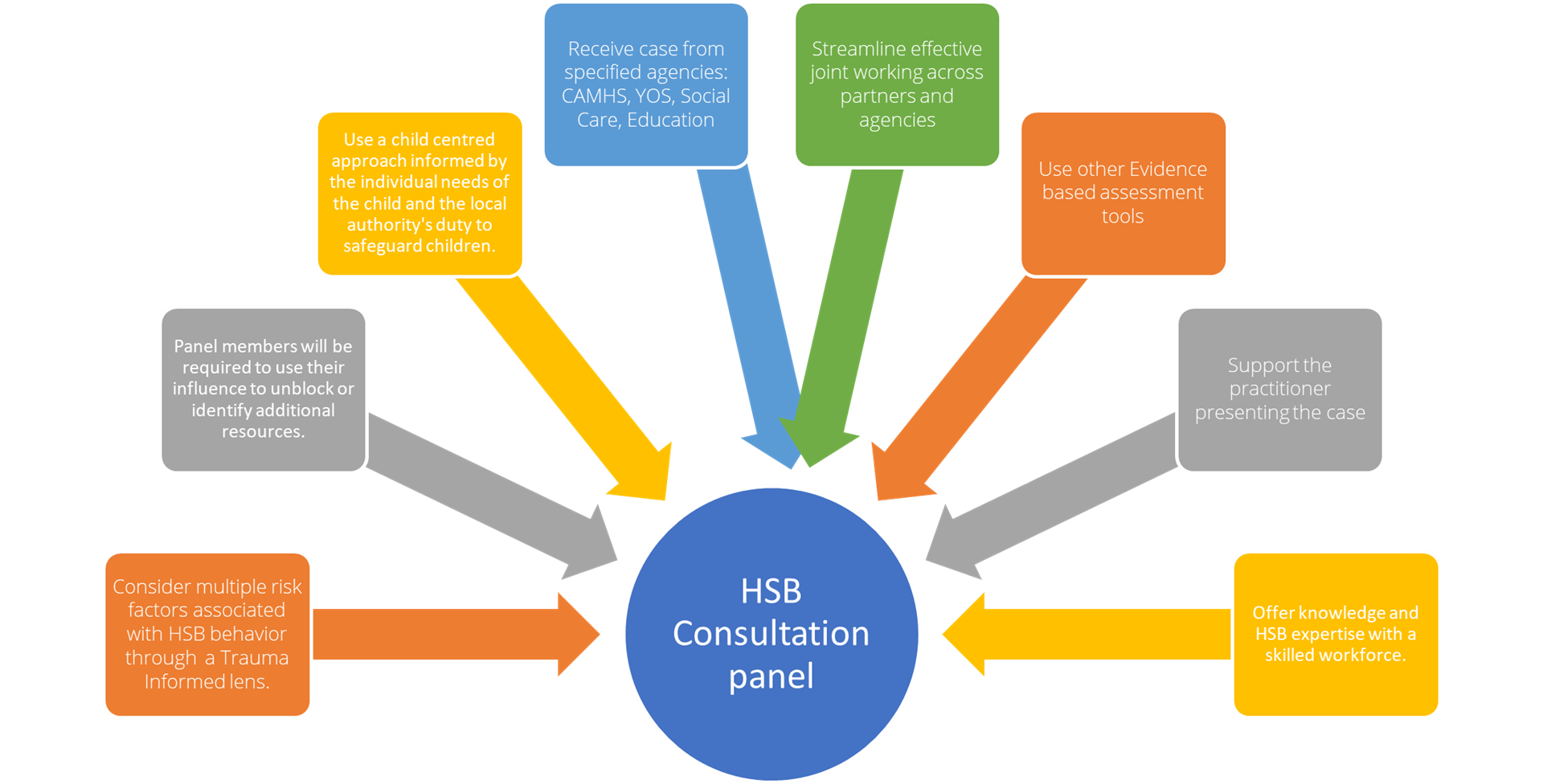
The consultation panel consists of multi-agency practitioners who are knowledgeable in the subject matter and may also be trained in the specialist AIM3 model.
What is A.I.M? +
The AIM (Assessment Intervention Moving on) project developed an assessment framework model in Manchester in 2000. The Framework was revised into AIM3 in 2007 and again in 2012, based on further research and evidence of young people aged 12-18 years. It is not an actuarial risk assessment tool, but an assessment framework designed to assist practitioners in the task of assessing HSB within the context of multiple domains of a young person’s life and identify the needs it is meeting. AIM3 has identified five domains: sexual behaviour, non-sexual behaviour developmental, environmental/family, and self-regulation.
AIM3 intends to be dynamic and responsive to developmental, systemic, and behavioural change.
More information about the assessment framework can be found here: https://aimproject.org.uk
Panel members +
Our agency partners & Panel members: +
Lewisham Youth Justice Service
 Alena Redwood
Alena Redwood
Advanced Practitioner,
Youth Justice Service
Lewisham Children Social care
 Tom Hatton,
Tom Hatton,
Team Manager in Lewisham
Family Support and Safeguarding service
|

Justine Mortlemans,
Group Manager in Lewisham
Family Support and Safeguarding service
|
South East London Integrated Care System (SEL ICS), Lewisham

Abimbola Adeyemi,
(Consultant Community Paediatrician & Designated Doctor for Safeguarding Children, South East London ICS Lewisham)
Primary Education

Julie Loffstadt,
Kilmorie Primary school
MET Police: Child Abuse Investigative Team (CAIT)

Keely Furness
Frequency of Panel Meetings +
The panel will meet every last Friday of the month at minimum (subject to change as the forum develops and service demands change).
Referrals +
Referrals will be considered from targeted and specialist agencies that are concerned about a young people who meets the criteria below.
Inclusion criteria for referrals concerning young people:
- Who have engaged in HSB resulting in significant harm to another child or young person.
- Are assessed as being likely to engage in HSB that would result in significant harm to themselves or others.
- All children under the age of 18 years for assessment and/or interventions.
- Panel may provide discretionary consultation for younger children.
Exclusion criteria for referrals concerning young people:
- Young people over the age of 18 years.
- No mention of HSB as the primary source of concerning behaviour.
- The HSB incident or the case has not been raised with Lewisham Children’s social care services.
- If the case is Child Sexual Exploitation in nature.
- Who are the victims of HSB?
Referrals will be:
- Submitted to the Chair via secure email by the beginning of the 3rd week of the month.
- Lead practitioners to provide a succinct written summary of the case and current safety plan for the young person and family.
- The ARTs team will have sole discretion over whether a referral is accepted or not into the forum. Where a referral is not accepted, the ARTs team will provide explanation as to why it is not accepted and signpost to other relevant services.
- In CAMHS cases, it will be expected that the referring practitioner will act as care co-ordinator for the case and team acting to support their work, with a more specialised assessment of risk and intervention
- Cases that are accepted for an AIM3 assessment, lead practitioners are expected to send the ARTs team appropriate assessment reports.
- AIM3 assessment will be carried out by two practitioners, which may be decided in the forum or between the ARTs team and other relevant agencies.
HSB Forum Consultation Request Form
Meeting Structure +
All presentations to the panel will be made by the lead practitioner. If the lead practitioner is unable to attend, their manager is expected to present the case on their behalf. To allow for an in-depth discussion each case will be allocated 60 minutes (subject to change as the forum develops). Once introductions have been completed, practitioners will have 10 to 15 minutes to present the case to the forum (i.e., what they would like to achieve from this consultation space, a brief overview of the presenting problem, family dynamics, what agencies are involved, and what the current safety plan is). The panel members will be invited to ask any clarifying questions, share reflections, identify any gaps in the case that need further consideration or what relevant information should be collated, and suggest possible interventions.
Quality assurance +
The ARTs team aim to audit the forum by keeping a log of cases discussed and collecting qualitative feedback from all lead practitioners who have presented at the forum via a Google feedback form.
Regular feedback will also be sought from the panel members to help improve the service design and delivery. The panel is dedicated to collecting and acting on feedback to ensure that the panel is a useful space to think about HSB cases with external partners and agencies.
Contact details +
For all referrals, inquiries or further information please email: artsteam@slam.nhs.uk
More information & Support +
Information Sharing & Consent
Contents
- Introduction
- London Multi-Agency Safeguarding Data Sharing Agreement for Safeguarding & Promoting the Welfare of Children - January 2021
- Principles of Information Sharing and Consent
- What is the Legal Framework that supports information sharing?
- Consent from a Young Person (Gillick Competence and Fraser Guidelines of Consent)
Appendix 1 – Data Protection Act 2018 Principles of Information Sharing
Appendix 2 – Information Sharing Flow Chart
Introduction
In order to ensure that safeguarding decisions are made with timely, necessary and proportionate interventions and support, decision makers require full information concerning children, their parents, carers and their circumstances to be available to them. Information viewed alone or in silos is unlikely to give the full picture or identify the true risks.
All relevant information from various agencies involved in their care or support, needs to be available and accessible in one place. A Multi-Agency Safeguarding Hub (MASH) helps ensure this and aids communication between all safeguarding partners, thus ensuring that the team quickly identifies those who are subject to or at risk of harm.
Information should only be shared within the MASH for the purposes of safeguarding and promoting the welfare of children, and for the prevention and detection of related crime.
HM Government advice on Information Sharing (May 2024)
This HM Government advice outlines the importance of sharing information about children, young people and their families in order to safeguard children. It should be read alongside the statutory guidance Working together to safeguard children 2023. The advice is non-statutory and replaces the HM Government Information sharing: advice for practitioners providing safeguarding services to children, young people, parents and carers published in July 2018.
This advice focuses on the legal framework and how it supports information sharing for the purposes of safeguarding children from abuse and neglect. It does not detail the additional professional responsibilities that might apply for different practitioners. Practitioners should consider this advice alongside guidance specific to their profession or service area. For example, doctors should consider the General Medical Council guidance, ‘Protecting Children and Young People and those working in schools and colleges should consider Keeping Children Safe in Education. Other relevant guidance documents, such as the Eight Caldicott principles, and useful materials can be found in Annex B.
This document includes information and advice regarding understanding safeguarding, understanding information sharing, understanding the "lawful" basis; the complexities of information sharing and consent, and why it causes confusion and your responsibilities regarding information sharing.
London Multi-Agency Safeguarding Data Sharing Agreement for Safeguarding & Promoting the Welfare of Children - January 2021 +
Local Safeguarding Partners are responsible for ensuring that relevant information is shared in a timely and proportionate way, both within the local area and across local authority boundaries. Local Safeguarding Partnerships should promote the use of the “London Multi-Agency Safeguarding Data Sharing Agreement for Safeguarding and Promoting the Welfare of Children” which sets out the legal basis for sharing information between agencies in London.
FAQs for Sharing Data Sharing Agreements
London Multi-Agency Safeguarding Data Sharing Agreement for Safeguarding & Promoting the Welfare of Children
Data Protection Impact Statement
The Seven Golden Rules for sharing information (including personal information)
- All children have a right to be protected from abuse and neglect. Protecting a child from such harm takes priority over protecting their privacy, or the privacy rights of the person(s) failing to protect them. The UK General Data Protection Regulation (UK GDPR) and the Data Protection Act 2018 (DPA) provide a framework to support information sharing where practitioners have reason to believe failure to share information may result in the child being at risk of harm.
- When you have a safeguarding concern, wherever it is practicable and safe to do so, engage with the child and/or their carer(s), and explain who you intend to share information with, what information you will be sharing and why. You are not required to inform them, if you have reason to believe that doing so may put the child at increased risk of harm (e.g., because their carer(s) may harm the child, or react violently to anyone seeking to intervene, or because the child might withhold information or withdraw from services).
- You do not need consent to share personal information about a child and/or members of their family if a child is at risk or there is a perceived risk of harm. You need a lawful basis to share information under data protection law, but when you intend to share information as part of action to safeguard a child at possible risk of harm, consent may not be an appropriate basis for sharing. It is good practice to ensure transparency about your decisions and seek to work cooperatively with a child and their carer(s) wherever possible. This means you should consider any objection the child or their carers may have to proposed information sharing, but you should consider overriding their objections if you believe sharing the information is necessary to protect the child from harm.
- Seek advice promptly whenever you are uncertain or do not fully understand how the legal framework supports information sharing in a particular case. Do not leave a child at risk of harm because you have concerns you might be criticised for sharing information. Instead, find out who in your organisation/agency can provide advice about what information to share and with whom. This may be your manager/supervisor, the designated safeguarding children professional, the data protection / information governance lead (e.g., Data Protection Officer), Caldicott Guardian, or relevant policy or legal team. If you work for a small charity or voluntary organisation, follow the NSPCC's safeguarding guidance.
- When sharing information, ensure you and the person or agency/organisation that receives the information take steps to protect the identities of any individuals (e.g., the child, a carer, a neighbour, or a colleague) who might suffer harm if their details became known to an abuser or one of their associates.
- Only share relevant and accurate information with individuals or agencies/organisations that have a role in safeguarding the child and/or providing their family with support, and only share the information they need to support the provision of their services. Sharing information with a third party rarely requires you to share an entire record or case-file – you must only share information that is necessary, proportionate for the intended purpose, relevant, adequate and accurate.
- Record the reasons for your information sharing decision, irrespective of whether or not you decide to share information. When another practitioner or organisation requests information from you, and you decide not to share it, be prepared to explain why you chose not to do so. Be willing to reconsider your decision if the requestor shares new information that might cause you to regard
information you hold in a new light. When recording any decision, clearly set out the rationale and be prepared to explain your reasons if you are asked.
Definitions
Personal Information/Data is:
- Information/Data which relates to a living, individual who can be identified from the data or other data/information that the organisation holds.
- Could be single elements or a combination e.g. names, addresses, occupation, date of birth etc.it could also include opinions about them and intentions towards them.
Sensitive Personal Information/Data is:
- Physical or mental health, racial or ethnic origin, political opinions, TU membership, sexual life, criminal allegations or record.
Principles of Information Sharing & Consent +
The principles set out below are intended to help practitioners working with children, young people, parents and carers share information between organisations. Practitioners should use their judgement when making decisions on what information to share and when and should follow organisation procedures or consult with their manager if in doubt. The most important consideration is whether sharing information is likely to safeguard and protect a child.
Necessary and proportionate
When taking decisions about what information to share, you should consider how much information you need to release. The Data Protection Act 2018 requires you to consider the impact of disclosing information on the information subject and any third parties. Any information shared must be proportionate to the need and level of risk.
Relevant
Only information that is relevant to the purposes should be shared with those who need it. This allows others to do their job effectively and make sound decisions.
Adequate
Information should be adequate for its purpose. Information should be of the right quality to ensure that it can be understood and relied upon.
Accurate
Information should be accurate and up to date and should clearly distinguish between fact and opinion. If the information is historical then this should be explained.
Timely
Information should be shared in a timely way to reduce the risk of harm. Timeliness is key in emergency situations and it may not be appropriate to seek consent for information sharing if it could cause delays and therefore harm to a child. Practitioners should ensure that sufficient information is shared, as well as consider the urgency with which to share it.
Secure
Information should be shared in the most secure way available. Practitioners must always follow their organisation’s policy on security for handling personal information.
Record
Information sharing decisions should be recorded whether or not the decision is taken to share. If the decision is to share, reasons should be cited including what information has been shared and with whom, in line with organisational procedures. If the decision is not to share, it is good practice to record the reasons for this decision and discuss them with the requester. Information should be kept In line with each organisation’s retention policy.
What Information can I share?
Share the information which is necessary for your purpose. It may not be necessary to give all agencies access to all the information you hold. Make sure what you provide is up to date, accurate and relevant.
When and how to share information
When asked to share information, you should consider the following questions to help you decide if and when to share. If the decision is taken to share, you should consider how best to effectively share the information.
When?
Q: Is there a clear and legitimate purpose for sharing information?
- Yes – see next question
- No – do not share information
Q: Does the information enable an individual to be identified?
- Yes – see next question
- No – you can share but should consider how
Q: Is the information confidential?
- Yes – see next question
- No – you can share but should consider how
Q: Do you have consent?
- Yes – you can share but should consider how
- No – see next question
Q: Is there another reason to share information such as to fulfil a public function or to protect the vital interests of the individual?
- Yes – you can share but should consider how
- No – do not share
Who?
- Which agencies need to be involved in the sharing?
- Who do we need information about in order to make the decision – child, parent, carer, others? Is it sensitive personal information? Do we have their consent?
How?
- Ensure you are giving the right information to the right person, and that it is shared securely.
- Identify how much information to share
- Distinguish fact from opinion
- Ensure that you are giving the right information to the right person
- Inform the individual that the information has been shared if they were not aware of this, as long as this would not create or increase risk of harm
Consent to Share Information
Check you have consent from all people whose information is to be shared unless the safeguarding concerns put the child at risk of significant harm or would prevent the child from being harmed. Ensure information shared is relevant and proportionate.
Agencies should be advised where possible to obtain consent before referring a case to the MASH Service. If this happens, individuals will have an understanding and expectation of how their information is going to be used, with whom and why. Where consent has not been obtained, reasons for this will be documented on both the agency and MASH records.
Where sensitive personal information is being shared explicit consent is expected, this may be written e.g. consent form or a clear record of verbal consent obtained stating the date, time and what information is to be held/shared.
In some cases, the work of the MASH might be obstructed if Partners were to seek consent. In such cases the disclosing Partner must consider other lawful basis for processing the information.
The decision whether or not to share information must be recorded by each partner agency.
Consider the following before sharing information - if in doubt seek advice from a manager
Consent
Do you have consent to share this information for this purpose? Consent is particularly important for sensitive personal information. The Privacy Notice (a statement that indicates consent to hold and share information see consent form) relating to the collection of information should identify the purposes for which it was collected. Does this say it would be shared? Otherwise consent should be obtained wherever possible before sharing information.
Partial Consent
Where consent has been given to share information with some, but not all, agencies, does this include the agency you want to share it with? If you do have consent, then the paragraph above applies. If you do not have consent, then the paragraph below applies.
Sharing without consent
If you are not seeking consent, the reason must be proportionate and you must weigh up the important legal duty to seek consent and the damage that might be caused by sharing the information. This should be balanced against the type and extent of any harm that might be caused (or not prevented) by seeking consent. It is good practice to obtain consent before sharing information. If consent is not obtained, the decision should always be reasonable, necessary and proportionate, and should always be recorded together with the rationale.
If the need to share is urgent, and seeking consent will lead to unjustified delay in making enquiries about allegations of significant harm to a child, or if safeguarding is paramount, take immediate action and share the information without consent, but remember to record the reason for the decision.
Sharing information when consent has been refused
There may be times when consent is sought and refused. This does not mean that information cannot be shared. The refusal of consent should be considered in conjunction with other concerns and, if it is considered justifiable, then information can and MUST be shared. If professionals consider it justifiable to override the refusal in the interests of the welfare of the child then they can do so. This decision must be proportionate to the harm that may be caused by proceeding without consent.
Public Interest
It is possible to disclose personal information without consent if this is in the defined category of “Public Interest”. The principles of the DPA [Section 2 above] would still apply in such cases.
The Public Interest Criteria include the:
- Protection of vulnerable members of the community
- Administration of justice
- Maintaining of public safety
- Apprehension of offenders
- Prevention of crime and disorder
- Detection of crime
- Protection of vulnerable members of the community
When judging the public interest, it is necessary to consider the following:
- Is the intended disclosure proportionate to the intended aim?
- What is the vulnerability of those who are at risk?
- What is the impact of disclosure likely to be on the individual to whom the shared information pertains?
- Is there another equally effective means of achieving the same aim?
- Is the disclosure necessary to prevent or detect crime and uphold the rights and freedoms of the public?
- Is it necessary to disclose the information, to protect others?
The rule of proportionality should be applied to ensure that a fair balance is achieved between the public interest and the rights of the individual’s information.
What is the Legal Framework that supports information sharing? +
The main legal framework relating to the protection of personal information is set out in:
There is no general power to obtain, hold or process information and there is no statutory power to share information. Where information is held it should be processed in accordance with the Data Protection Act principles.
However, some Acts of Parliament do give statutory public bodies express or implied statutory powers to share information under some circumstances. There are a number of pieces of legislation. Some of these are relevant to all members of the Family Safeguarding Teams. Others relate to specific organisations.
Legislation allows the lawful sharing of personal information and is covered in this guide using the following legislative frameworks.
Working Together 2023 states that:-
28. No single practitioner can have a full picture of a child’s needs and circumstances so effective sharing of information between practitioners, local organisations and agencies is essential for early identification of need, assessment, and service provision to keep children safe. Rapid reviews and child safeguarding practice reviews have highlighted that missed opportunities to record, understand the significance of, and share information in a timely manner can have severe consequences for children.
29. Practitioners should be proactive in sharing information as early as possible to help identify, assess, and respond to risks or concerns about the safety and welfare of children. This may be when problems are first emerging (for example, persistent school absences) or where a child is already known to local authority children’s social care. Sharing information about any adults with whom that child has contact, which may impact the child’s safety or welfare, is also critical.
30. Information sharing is also essential for the identification of patterns of behaviour when a child is at risk of going missing or has gone missing, including being missing from education. When multiple children appear associated to the same context or locations of risk, or in relation to children in the secure estate where there may be multiple local authorities involved in a child’s care, it will be for local safeguarding partners to consider how they build relationships and share relevant information in a timely and proportionate way with each other, other local organisations, and other safeguarding partnerships.
31. The Data Protection Act 201812 and UK General Data Protection Regulation (UK GDPR) supports the sharing of relevant information for the purposes of keeping children safe. Fears about sharing information must not be allowed to stand in the way of safeguarding and promoting the welfare of children. To ensure effective safeguarding arrangements:
- all organisations and agencies should have arrangements in place that set out clearly the processes and the principles for sharing information. The arrangements should cover how information will be shared with their own organisation/agency and with others who may be involved in a child’s life
- practitioners should not assume that someone else will pass on information that they think may be critical to keep a child safe. If a practitioner has concerns about a child’s welfare or safety, then they should share the information with local authority children’s social care and/or the police. All practitioners should be particularly alert to the importance of sharing information when a child moves from one local authority into another, due to the risk that knowledge pertinent to keeping a child safe could be lost
- UK GDPR provides a number of bases for sharing personal information. It is not necessary to seek consent to share information for the purposes of safeguarding and promoting the welfare of a child provided that there is a lawful basis to process any personal information required. The legal bases that may be appropriate for sharing data in these circumstances could be “legal obligation” or “public task”, which includes the performance of a task in the public interest or the exercise of official authority. Each of the lawful bases under UK GDPR has different requirements13. In some circumstances, it may be appropriate to obtain consent to share data, but it is important to note that UK GDPR sets a high standard for consent which is specific, time limited and can be withdrawn (in which case the information would have to be deleted).
32. Practitioners must have due regard to the relevant data protection principles which allow them to share personal information, as provided for in the Data Protection Act 2018 and UK GDPR. To share information effectively:
- practitioners should be confident of the lawful bases and processing conditions under the Data Protection Act 2018 and UK GDPR that allow them to store and share information, including information which is considered sensitive, such as health data, known under the data protection legislation as “special category personal data”
- where practitioners need to share special category personal data, for example, where information obtained is sensitive and needs more protection, they should consider and identify the lawful basis for doing so under Article 6 of UK GDPR, and in addition be able to meet one of the specific conditions for processing under Article 9. The Data Protection Act 2018 specifies “safeguarding of children and individuals at risk” as a processing condition that allows practitioners to share information, including without consent (where in the circumstances consent cannot be given, it cannot be reasonably expected that a practitioner obtains consent or if to gain consent would place a child at risk). However, practitioners should be aware of the risks of processing special category data and be mindful that a data protection impact assessment must be completed for any type of processing which is likely to be high risk.
Practitioners should aim to be as transparent as possible by telling families what information they are sharing and with whom, provided that it is safe to do so.
Myth Busting Guide
Sharing information enables practitioners and agencies to identify and provide appropriate services that safeguard and promote the welfare of children. Below are common myths that may hinder effective information sharing:-
Data Protection legislation is a barrier to sharing information
NO. The Data Protection Act 2018 and GDPR do not prohibit the collection and sharing of personal information, but rather provides a framework to ensure that personal information is shared appropriately. In particular, the Data Protection Act 2018 balances the rights of the information subject (the individual whom the information is about) and the possible need to sharing information about them.
Consent is needed to share personal information
NO You do not need consent to share personal information. It is one way to comply with the data protection legislation but not the only way. UK GDPR provides a number of bases for sharing personal information. It is not necessary to seek consent to share information for the purposes of safeguarding and promoting the welfare of a child provided that there is a lawful basis to process any personal information required. The legal bases that may be appropriate for sharing data in these circumstances could be ‘legal obligation’, or ‘public task’ which includes the performance of a task in the public interest or the exercise of official authority. Each of the lawful bases under UK GDPR has different requirements. It is good practice to be transparent and inform parents/carers that you are sharing information for these purposes and seek to work cooperatively with them, where it is safe to do so.
Personal information collected by one organisation / agency cannot be disclosed to another
NO This is not the case unless the information is to be used for a purpose incompatible with the purpose for which it was originally collected. In the case of children in need, or children at risk of significant harm, it is difficult to foresee circumstances where information law would be a barrier to sharing personal information with other practitioners.
The common law duty of confidence and the Human Rights Act 1998 prevent the sharing of personal information
NO No, this is not the case. In addition to the Data Protection Act 2018 and GDPR, practitioners need to balance the common law duty of confidence and the Human Rights Act 1998 against the effect on individuals or others of not sharing the information
IT systems are often a barrier to effective information sharing
There are many IT systems that support the sharing of information, such as the Child Protection Information Sharing project (CP-IS). It is important that the sector continues to work with IT suppliers to ensure that their user needs around information sharing are factored into priorities for system enhancement..
Data Protection Act 2018
Everyone responsible for using personal data has to follow strict rules called ‘data protection principles’. They must make sure the information is:
- used fairly, lawfully and transparently
- used for specified, explicit purposes
- used in a way that is adequate, relevant and limited to only what is necessary
- accurate and, where necessary, kept up to date
- kept for no longer than is necessary
- handled in a way that ensures appropriate security, including protection against unlawful or unauthorised processing, access, loss, destruction or damage
There is stronger legal protection for more sensitive information, such as:
- race
- ethnic background
- political opinions
- religious beliefs
- trade union membership
- genetics
- biometrics (where used for identification)
- health
- sex life or orientation
There are separate safeguards for personal data relating to criminal convictions and offences.
Data Protection Act (DPA) 2018: The principles of the DPA 2018 provide a framework within which to consider the lawful basis for sharing information under this agreement. Data Protection Act Key Principles can be read by CLICKING HERE or viewed on Appendix A at the end of this page.
Each partner agency may have a different reason for holding and processing the information it needs to fulfil its legal duties. Some common considerations have been included here, but it is impossible to cover all possible situations. Partner agencies must obtain their own assurance and be satisfied that they have a lawful basis for sharing the information they hold.
DPA Section 29 This section provides certain exemptions when personal information is used for the prevention and detection of crime and/or for the apprehension and prosecution of offenders. For example, telling individuals how their information will be processed or shared could prejudice the purpose. Note that information processed for this purpose is exempt from disclosure in response to a Subject Access Request.
Children Act 2004
Sections 10 and 11 of the Children Act 2004 place obligations upon agencies including local authorities, police, clinical commissioning groups and NHS England to co-operate with other partners in promoting the welfare of children and ensuring that they act safeguard and promote the welfare of children in their area.
Well‐being is defined by the Act as relating to a child’s:
- Physical and mental health and emotional well‐being
- Protection from harm and neglect
- Education, training and recreation
- The contribution made by them to society
- Social and economic well‐being
‘Children’ in terms of the scope of this Act means those up to the age of eighteen.
Children Act 1989
For children and young people, the nature of the information that will be shared within the MASH may fall below a statutory threshold of Section 47 (children in need of protection) or even Section 17 (children in need of services).
Crime and Disorder Act 1998
Provides a legal basis for sharing information with a relevant authority where the disclosure is necessary or expedient for the purposes of any provision of the Crime and Disorder Act 1998. Relevant authorities include: Police, Probation, Local Authorities, CCGs and certain NHS statutory bodies
Human Rights Act 1998
Gives force to the European Convention on Human Rights and, amongst other things, places an obligation on public authorities to protect people’s “right to life” and “right to be free from torture or degrading treatment”.
There needs to be a balance between the desire to share and a person’s right to privacy under “the right to respect for private and family life, home and correspondence”. The local authority cannot interfere with this right except such as is necessary in the interests of national security, public safety or for the prevention of disorder or crime, for the protection of health and wellbeing, or for the protection of the rights and freedoms of others.
The Mental Capacity Act (MCA) 2005.
Under the Mental capacity Act 2005 staff are required to apply five principles in their assessments to decide whether to share information without consent in a person’s best interests.
The MCA Code of Practice states that “it is important to balance people's right to make a decision with their right to safety and protection when they can't make decisions to protect themselves. The starting assumption must always be that an individual has the capacity, until there is proof that they do not”.
Under the Mental Capacity Act 2005 there would have to be good reasons not to undertake an assessment of mental capacity regarding the decision to share information without consent. These reasons would need to be documented carefully.
Counter-Terrorism and Boarder Security Act 2019
The Counter Terrorism and Security Act 2015 places a duty on “specified authorities” to have “due regard to the need to prevent people from being drawn into terrorism”. Specified authorities include County and District/Borough Councils, Schools; Police; National Probation Service and Community Rehabilitation Companies; NHS Trusts and NHS Foundation Trusts.
Prevent Duty Guidance
The Prevent Strategy has three specific strategic objectives:
- respond to the ideological challenge of terrorism and the threat we face from those who promote it;
- prevent people from being drawn into terrorism and ensure that they are given appropriate advice and support; and
- Work with sectors and institutions where there are risks of radicalisation that we need to address.
There is an expectation that authorities will work in partnership and share information where appropriate, for example to ensure someone at risk of radicalisation is supported.
Duty of Confidence Information shared by agencies as part of the MASH assessment process may have been gathered where a Duty of Confidence is owed. A duty of confidence arises when one person discloses information to another in circumstances where it is reasonable to expect that the information will not be further disclosed. Duty of Confidence is not an absolute bar to disclosure, as information can be shared where there is a strong enough public interest to do so.
When overriding the Duty of Confidence in the absence of consent, MASH must seek the views of the person representing the organisation that holds the Duty of Confidence and take these into account in relation to breaching the confidence. The originating Partner will be the final arbiter as to whether information is disclosed or not. The Partner may wish to seek specialist or legal advice if there is lack of clarity around justifiable disclosure of information. All disclosures must be relevant and proportionate to the intended aim of the disclosure and must be fully documented as an unjustified disclosure could lead to a claim for damages against the disclosing party.
All staff must be particularly mindful of their professional and ethical obligations and the public interest of confidence in the confidentiality of their services.
It may be necessary to seek advice on professional conduct as well as legal advice before sharing information without consent, especially for information related to the treatment of mental illness. All staff should ensure the need to protect children takes into account the children’s rights as well as those of the adults concerned. Decisions will be reported to the MASH Executive Group for periodic review.
Gillick competency and Fraser guidelines help people who work with children to balance the need to listen to the children’s wishes with the responsibility to keep them safe.
When practitioners are trying to decide whether a child is mature enough to make decisions about things that affect them, they often talk about whether the child is “Gillick competent” or whether they need the “Fraser guidelines”.
Although the two terms are frequently used together and originate from the same legal case, there are distinct differences between them.
Both Gillick competency and Fraser guidelines refer to a legal case from the 1980s which looked at whether doctors should be able to give contraceptive advice or treatment to young people under 16-years-old without parental consent.
Applying Gillick competence and Fraser Guidelines
The Fraser guidelines still apply to advice and treatment relating to contraception and sexual health. But Gillick competency is often used in a wider context to help assess whether a child has the maturity to make their own decisions and to understand the implications of those decisions. Practitioners should always encourage a child to tell their parents or carers about the decisions they are making. If they don’t want to do this, you should explore why and, if appropriate, discuss ways you could help them inform their parents or carers. For example, you could talk to the young person’s parents or carers on their behalf.
If the young person still wants to go ahead without their parents’ or carers’ knowledge or consent, you should consider the Gillick and Fraser guidelines.
Gillick Competence
Gillick competency applies mainly to medical advice but it is also used by practitioners in other settings. For example, if a child or young person:-
- Would like to have counselling or therapeutic support but doesn’t want their parents or carers to know about it.
- Is seeking confidential support for substance misuse.
- Has strong wishes about their future living arrangements which may conflict with their parents’ or carers’ views.
Medical professionals need to consider Gillick competency if a young person under the age of 16 wishes to receive treatment without their parents’ or carers’ consent or, in some cases, knowledge.
If the young person has informed their parents of the treatment they wish to receive but their parents do not agree with their decision, treatment can still proceed if the child has been assessed as Gillick competent.
Assessing Gillick Competence
There is not set of defined questions to assess Gillick competency. Professionals need to consider several things when assessing a child’s capacity to consent, including:
- The child’s age, maturity and mental capacity
- Their understanding of the issue and what it involves – including advantages, disadvantages and potential long-term impact.
- Their understanding of the risks, implications and consequences that may arise from their decision.
- How well they understand any advice or information they have been given.
- Their understanding of any alternative options, if available.
- Their ability to explain a rationale around their reasoning and decision making.
Remember that consent is not valid if a young person is pressured or influenced by someone else.
Children’s capacity to consent may be affected by different factors, for example stress, mental health conditions and the complexities of the decision they are making. The same child may be considered Gillick competent to make one decision but not competent to make a different decision.
If you don’t think a child is Gillick competent or there are inconsistencies in their understanding, you should seek consent from their parents or carers before proceeding.
In complex medical cases, such as those involving disagreements about treatment, you may wish to seek the opinion of a colleague about a child’s capacity to consent (Care Quality Commission 2019)
Young people also have the right to seek a second opinion from another medical professional (General Medical Council, 2020).
Refusal of Medical Treatment
Gillick competency can be used when young people wish to use medical treatment. However, if a young person refuses medical treatment which may lead to their death or severe permanent harm, their decision can be overruled. More information about this is available in the Guidance for Medical Professionals in each UK nation – see case history and legislation on the NSPCC website.
Child Protection Concerns
The child’s safety and wellbeing is paramount.
When you are assessing Gillick competency if you have any concerns about the safety of the young person you should check whether previous child protection concerns have been raised, and explore any factors that could put them at risk of abuse.
You must always share child protection concerns with the relevant agencies, even if this goes against a child’s wishes. (Find out more on Recognising & Responding to Abuse, NSPCC).
Fraser Guidelines
The Fraser guidelines apply specifically to advice and treatment about contraception and sexual health. They may be used by a range of healthcare professionals when working with under 16 year-olds, including doctors and nurse practitioners.
Following a legal ruling in 2006, Fraser guidelines can also be applied to advice and treatment for sexually transmitted infections and the termination of pregnancy (Axton v the Secretary of Stage for Health, 2006).
Using the Fraser guidelines
Practitioners using the Fraser guidelines should be satisfied of the following:
- The young person cannot be persuaded to inform their parents or carers that they are seeking this advice or treatment (or to allow the practitioner to inform their parents or carers).
- The young person understands the advice being given.
- The young person’s physical or mental health (or both) are likely to suffer unless they receive the advice or treatment.
- It is in the young person’s best interests to receive the advice, treatment or both without their parents’ or carers’ consent.
- The young person is very likely to continue having sex with or without contraceptive treatment.
Child Protection Concerns
When using Fraser guidelines for issues relating to sexual health, you should always consider any potential child protection concerns:
- Underage sexual activity is a possible indicator of child sexual exploitation and children who have been groomed may not realise they are being abused.
- Sexual activity with a child under 13 should always result in a child protection referral.
- If a young person presents repeatedly about sexually transmitted infections or the termination of pregnancy this may be an indicator of child sexual abuse or exploitation.
Professionals should always consider any previous concerns that may have been raised about the young person and explore whether there are any factors that may present a risk to their safety and wellbeing.
You must always share child protection concerns with the relevant agencies, even if a child or young person asks you not to.
Appendix 1 – Data Protection Act 2018 Principles of Information Sharing +
CHAPTER 2 Principles Overview and general duty of controller
(1)This Chapter sets out the six data protection principles as follows—
(a) section 35(1) sets out the first data protection principle (requirement that processing be lawful and fair);
(b) Section 36(1) sets out the second data protection principle (requirement that purposes of processing be specified, explicit and legitimate);
(c) Section 37 sets out the third data protection principle (requirement that personal data be adequate, relevant and not excessive);
(d) Section 38(1) sets out the fourth data protection principle (requirement that personal data be accurate and kept up to date);
(e) Section 39(1) sets out the fifth data protection principle (requirement that personal data be kept for no longer than is necessary);
(f) Section 40 sets out the sixth data protection principle (requirement that personal data be processed in a secure manner).
(2) In addition—
(a) Each of sections 35, 36, 38 and 39 makes provision to supplement the principle to which it relates, and
(b) Sections 41 and 42 make provision about the safeguards that apply in relation to certain types of processing.
(3) The controller in relation to personal data is responsible for, and must be able to demonstrate, compliance with this Chapter.
The first data protection principle
(1) The first data protection principle is that the processing of personal data for any of the law enforcement purposes must be lawful and fair.
(2) The processing of personal data for any of the law enforcement purposes is lawful only if and to the extent that it is based on law and either—
(a) The data subject has given consent to the processing for that purpose, or
(b) The processing is necessary for the performance of a task carried out for that purpose by a competent authority.
(3) In addition, where the processing for any of the law enforcement purposes is sensitive processing, the processing is permitted only in the two cases set out in subsections (4) and (5).
(4) The first case is where—
(a) The data subject has given consent to the processing for the law enforcement purpose as mentioned in subsection (2)(a), and
(b) At the time when the processing is carried out, the controller has an appropriate policy document in place (see section 42).
(5) The second case is where—
(a) The processing is strictly necessary for the law enforcement purpose,
(b) The processing meets at least one of the conditions in Schedule 8, and
(c) At the time when the processing is carried out, the controller has an appropriate policy document in place (see section 42).
(6) The Secretary of State may by regulations amend Schedule 8—
(a) By adding conditions;
(b) By omitting conditions added by regulations under paragraph (a).
(7) Regulations under subsection (6) are subject to the affirmative resolution procedure.
(8) In this section, “sensitive processing” means—
(a) The processing of personal data revealing racial or ethnic origin, political opinions, religious or philosophical beliefs or trade union membership;
(b) The processing of genetic data, or of biometric data, for the purpose of uniquely identifying an individual;
(c) The processing of data concerning health;
(d) The processing of data concerning an individual’s sex life or sexual orientation.
The second data protection principle
(1)The second data protection principle is that—
(a) The law enforcement purpose for which personal data is collected on any occasion must be specified, explicit and legitimate, and
(b) Personal data so collected must not be processed in a manner that is incompatible with the purpose for which it was collected.
(2) Paragraph (b) of the second data protection principle is subject to subsections (3) and (4).
(3) Personal data collected for a law enforcement purpose may be processed for any other law enforcement purpose (whether by the controller that collected the data or by another controller) provided that—
(a) The controller is authorised by law to process the data for the other purpose, and
(b) The processing is necessary and proportionate to that other purpose.
(4) Personal data collected for any of the law enforcement purposes may not be processed for a purpose that is not a law enforcement purpose unless the processing is authorised by law.
The third data protection principle
The third data protection principle is that personal data processed for any of the law enforcement purposes must be adequate, relevant and not excessive in relation to the purpose for which it is processed.
The fourth data protection principle
(1) The fourth data protection principle is that—
(a) Personal data processed for any of the law enforcement purposes must be accurate and, where necessary, kept up to date, and
(b) Every reasonable step must be taken to ensure that personal data that is inaccurate, having regard to the law enforcement purpose for which it is processed, is erased or rectified without delay.
(2) In processing personal data for any of the law enforcement purposes, personal data based on facts must, so far as possible, be distinguished from personal data based on personal assessments.
(3) In processing personal data for any of the law enforcement purposes, a clear distinction must, where relevant and as far as possible, be made between personal data relating to different categories of data subject, such as—
(a) Persons suspected of having committed or being about to commit a criminal offence;
(b) Persons convicted of a criminal offence;
(c) Persons who are or may be victims of a criminal offence;
(d) Witnesses or other persons with information about offences.
(4) All reasonable steps must be taken to ensure that personal data which is inaccurate, incomplete or no longer up to date is not transmitted or made available for any of the law enforcement purposes.
(5) For that purpose—
(a) The quality of personal data must be verified before it is transmitted or made available,
(b) In all transmissions of personal data, the necessary information enabling the recipient to assess the degree of accuracy, completeness and reliability of the data and the extent to which it is up to date must be included, and
(c) If, after personal data has been transmitted, it emerges that the data was incorrect or that the transmission was unlawful, the recipient must be notified without delay.
The fifth data protection principle
(1) The fifth data protection principle is that personal data processed for any of the law enforcement purposes must be kept for no longer than is necessary for the purpose for which it is processed.
(2) Appropriate time limits must be established for the periodic review of the need for the continued storage of personal data for any of the law enforcement purposes.
The sixth data protection principle
The sixth data protection principle is that personal data processed for any of the law enforcement purposes must be so processed in a manner that ensures appropriate security of the personal data, using appropriate technical or organisational measures (and, in this principle, “appropriate security” includes protection against unauthorised or unlawful processing and against accidental loss, destruction or damage).
Safeguards: archiving
(1) This section applies in relation to the processing of personal data for a law enforcement purpose where the processing is necessary
(a) For archiving purposes in the public interest,
(b) For scientific or historical research purposes, or
(c) For statistical purposes.
(2) The processing is not permitted if—
(a) It is carried out for the purposes of, or in connection with, measures or decisions with respect to a particular data subject, or
(b) It is likely to cause substantial damage or substantial distress to a data subject.
42Safeguards: sensitive processing
(1) This section applies for the purposes of section 35(4) and (5) (which require a controller to have an appropriate policy document in place when carrying out sensitive processing in reliance on the consent of the data subject or, as the case may be, in reliance on a condition specified in Schedule 8).
(2) The controller has an appropriate policy document in place in relation to the sensitive processing if the controller has produced a document which—
(a) Explains the controller’s procedures for securing compliance with the data protection principles (see section 34(1)) in connection with sensitive processing in reliance on the consent of the data subject or (as the case may be) in reliance on the condition in question, and
(b) Explains the controller’s policies as regards the retention and erasure of personal data processed in reliance on the consent of the data subject or (as the case may be) in reliance on the condition in question, giving an indication of how long such personal data is likely to be retained.
(3) Where personal data is processed on the basis that an appropriate policy document is in place, the controller must during the relevant period—
(a) Retain the appropriate policy document,
(b) Review and (if appropriate) update it from time to time, and
(c) Make it available to the Commissioner, on request, without charge.
(4) The record maintained by the controller under section 61(1) and, where the sensitive processing is carried out by a processor on behalf of the controller, the record maintained by the processor under section 61(3) must include the following information—
(a) Whether the sensitive processing is carried out in reliance on the consent of the data subject or, if not, which condition in Schedule 8 is relied on,
(b) How the processing satisfies section 35 (lawfulness of processing), and
(c) Whether the personal data is retained and erased in accordance with the policies described in subsection (2)(b) and, if it is not, the reasons for not following those policies.
(5) In this section, “relevant period”, in relation to sensitive processing in reliance on the consent of the data subject or in reliance on a condition specified in Schedule 8, means a period which—
(a) Begins when the controller starts to carry out the sensitive processing in reliance on the data subject’s consent or (as the case may be) in reliance on that condition, and
(b) Ends at the end of the period of 6 months beginning when the controller ceases to carry out the processing.
Appendix 2 – Information Sharing Flow Chart +
Keeping Babies Safe
We aim to raise awareness and encourage discussions with parents and care givers around safe sleeping arrangements and preventing injuries in babies. Even if this is not your service target age group, good practice suggests that where we notice a pregnant mother or infant of 0-2 we have an opportunity to talk about keeping babies safe.
Please also see our Parents Safe Sleep Advice Page (information provided by the Lullaby Trust). This is transferable to all known languages using the Google Language tool at the top of the website.
Preventing Sudden Unexplained Death in Infancy (SUDI) +
A number of Child Safeguarding Practice Reviews centre around infants aged 0-2 years who have died by way of Sudden Unexplained Death in Infancy (SUDI).
Safe Sleep for Babies
Preventing Sudden Infant Death Syndrome / Sudden Unexplained Death in Infants
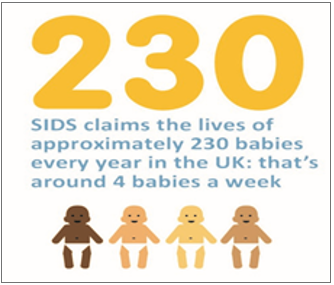 |
14 Babies died with an initial diagnosis of SUDI in Bexley, Greenwich and Lewisham between December 2020 and December 2022.
These are previously healthy babies - please help prevent the tragic deaths of children by making sure you know the Key Facts when discussing safe sleeping with parents
|
Below provides some insight to SUDI Deaths and their Associated Risk Factors in Lewisham from 2008 to 2022, with the Tri-Borough numbers being included from October 2019.
- 24 Boys and 11 Girls have died of Sudden Unexpected Death in Infancy (SUDI) / Sudden Infant Death Syndrome (SIDS) since 2008
- Room temperature above 20 °C was noted in 79% of cases where room temperature was measured.
- Room temperature was not being measured routinely in a high number of earlier SUDI’s, though that has now been rectified. In the 19 SUDI cases where room temperature was measured, 15 found a room temperature of above 20 °C. (the recommended temperature is between 16-20 °C)
- Poverty / Overcrowding (57%)
- Excess Bedding-pillows, duvets (53%)
- Bed sharing with at least 1 other risk factor (48%)
- Parental Smoking (37%)
|
- Baby put to sleep or found on side or prone position (32%)
- The number of babies laid to sleep on their side or prone has increased in the last year
- Low birth rate of under 2.5kgs (26%)
- Parental Alcohol (20%)
- Language and Communication Issues, Learning Disability / Ability. (17%)
- Pre-Term Baby <37 weeks gestation. (17%)
- Mother is 20 years old or younger. (14%)
- Sofa Sleeping (9%)
- Parental use of Cannabis (6%)
- No cases of SUDI when mother was exclusively breastfeeding and bed sharing with no other risk factors.
|
Tri-Borough Public Health : Key Facts
Things parents can do to help prevent SUDI/SIDS:
|
Things to avoid:
|
|

|
Always place baby on their back to sleep-if they roll on to tummy, move them back
|

|
Avoid letting your baby get too hot. The room temperature should be between 16-20 degrees. If your baby is sweating or their tummy feels hot to the touch, take off some of the bedding or clothing.
|
|

|
Breastfeed your baby if you can as breastfeeding is highly protective
|

|
Never sleep on a sofa or armchair with your baby-this is particularly unsafe and significantly increases the risk of a SUDI death
|
|

|
Keep your home and therefore your baby smoke free in pregnancy and afterwards
|

|
Don’t cover your baby’s face or head whilst sleeping
|
|

|
Place your baby to sleep in a separate cot or Moses basket in the same room as you for the first six months.
|

|
Don’t sleep in the same bed as your baby if either of you have smoked, have been drinking any alcohol, have taken drugs, are extremely tired or if your baby was born prematurely or was of low birth-weight (under 5lbs 8oz)
|
|

|
Place your baby in the "feet to foot" position (with their feet at the end of the cot or Moses basket)
|

|
Parents/carers smoking increase risks to babies and children-ask Midwife/Health Visitor/GP/online for support to quit
|
|

|
Use a firm, flat waterproof mattress in good condition-remove any plastic covering
|

|
Remove all pillows, duvets, cot bumpers and soft toys from the cot and sleeping area
|
|

|
If you are planning to visit friends/relatives or stay away from home, make a plan as to how you will keep the baby’s sleep area safe
|
|
|
Check Understanding!

We have had a significant number of deaths in cases where either the mother speaks and understands limited English or where she is dyslexic or described as having a, ‘mild learning disability’.
- It is important to use an interpreter when discussing safe sleep if English is not a parents first language.
- Consideration should also be given if the mother or father has information processing issues, ask her/him to show you and explain back to you how to sleep the baby safely.
- You can use the LSCP Safe Sleep for Babies web page, The website can be transferred into all known languages and can be a useful tool.
There are good resources for parents, including visual aids and information in 16 different languages on the following website www.lullabytrust.org.uk
Professionals working with new or expectant parent(s) should be mindful of the impact of financial pressures on family budgets (poverty, low income, cost of living increases, child care costs) and how this may impact on the parent(s) ability to accesses equipment for babies.
All agencies should consider what resource’s they can access to support families who need help to get necessary baby equipment,this can include direct support or referring to other organisations including the voluntary sector.
Resources for parents who may need support or equipment for their baby
- Parents who need extra support can obtain a free thermometer from their Midwife.
- The Lewisham Donation Hub, Unit D Place Ladywell, 261 Lewisham High Street, SE13 6AY Lewisham Donation Hub – Supporting our community since 2020
- Little Village. the referral must be made by a professional Home - Little Village (littlevillagehq.org)
- Apply to BBC Children in Need fund Grants - BBC Children in Need
- Home - Buttle UK
Awareness Resources / Posters to Support the Campaign
To support the Keeping Babies Safe Campaign, the LSCP have developed a public facing Safe Sleep poster for partners to place in prominent areas. You can download the LSCP Poster HERE.
Additionally, the Lullaby Trust have a series of public facing posters that can be placed in public facing areas. Please use as many as you can, or rotate them periodically.
For more resources of leaflets, easy read cards and posters visit www.lullabytrust.org.uk

Preventing Non-Accidental Injuries and Shaken Baby Syndrome in Infant Years +
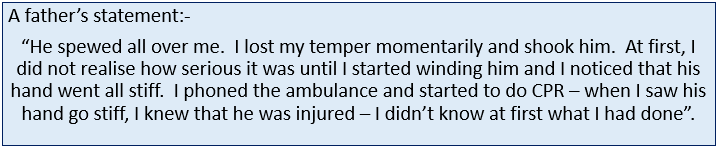
Overview
A number of Child Safeguarding Practice Reviews centre around infants aged 0-2 years, who have died or suffered significant harm, by way of non-accidental injury / shaken baby.
Over recent years, the Tri-Borough have identified a number of children who have attended A&E where either of these have been a factor.
Additionally, in relation to this the NSPCC have also published a report “The Myth of Invisible Men: Safeguarding children under 1 from non-accidental injury caused by male carers”.
We aim to raise awareness and encourage discussions with parents and carers around coping with crying and non-accidental injuries to infants.

Parents & Carers can download the ICON Cope Application on their App Store / Google Play Store on their device(s)
|
Awareness Resources / Posters
ICON have a series of public facing posters. Please use as many as you can, or rotate them periodically.
For more resources of leaflets, easy read cards and posters visit www.iconcope.org
The Myth of Invisible Men: Safeguarding children under 1 from non-accidental injury caused by male carers – KEY FINDINGS
- Perinatal neonaticides (homicides within 24hrs of birth) are almost exclusively perpetrated by birth mothers.
- Between 2000 and 2015 in England and Wales, 122 babies were killed by fathers (11 of these by step-fathers) giving an average of eight infants per year killed. Of these, 31 died as a consequence of shaking.
- In the only UK analysis we found, covering convicted homicides in England and Wales over the period 1997-2006, infants were more likely to be killed by a father (as the main perpetrator) than by a mother in the approximate ratio 2:1.9
- Biological fathers are more likely to kill infants than stepfathers in ratios ranging from 5:1 to 26.1 in the first year of life in the UK, USA, Australia and New Zealand.
- The ratio of biological fathers to ‘stepfathers’ (including mothers’ non-cohabiting and short-term partners) where babies have been killed in England and Wales is 10:1. This increases to 15:1 when shaking is the cause of death.
- However, when factoring in the very small proportion of infants with a stepfather, the evidence suggests that stepfathers are associated with greater risk than birth fathers. The numbers are lower but the risks are greater.
- The ratio of biological fathers to ‘stepfathers’ evened out or reversed for father-perpetrated homicide of older babies and pre-school children aged 1 to 5 years in England and Wales.
- When the research scope was broadened to look at non-fatal NAI, a clear picture emerges. Fathers outnumbered mothers as perpetrators of identified abuse head trauma (AHT), and this is a consistent finding in international data with the fathers to mothers ratio ranging from 2:1 to 10:1.
- There is also noteworthy data about the gender of babies abused. A consistent and well-evidenced finding from the literature review is that sons are more likely than daughters to be victims of father-perpetrated NAI. The one large international study that includes this data found that boys outnumbered girl victims 56% to 44%; even where mothers had been the identified perpetrator, boys were more likely to be victims than girls (53% boys compared to 47% girls).
- In the cohort of cases for this review, 57% were boys and 43% were girls. In the much smaller sample of men that were interviewed boy victims outnumbered girls 2:1. At this stage, and without further research, it is not possible to draw any specific conclusions, but the difference is of note and warrants further enquiry.
Bruising Protocol for Non-independently Mobile Infants & Children +
Introduction
Bruising is strongly related to mobility and once children are mobile, they can sustain bruises through everyday activities and accidents. Bruising in an infant who is pre-mobile is, however, very unusual and should always be investigated. Local and national Child Safeguarding Practice Reviews have identified the need for heightened concern when bruises are seen in infants without independent mobility. It is nationally recognised that pre-mobile infants are at greater risk of abuse than older children. Children with disabilities are more likely to be abused than non-disabled infants.
There is an information leaflet for parents/ carers in addition to the protocol. The information leaflet is given to the parents/carers at the hospital by a clinician following medical investigation. This leaflet is intended to aid conversation between clinicians and parents/carers and should be used as a tool to help with communication.
For the purposes of this pathway the terminology “infant” will be used and will be defined as being from ages 0 -12 months.
The Child Safeguarding Practice Review (CSPR) Panel issued a briefing in September 2022, ’Bruising in non-mobile infants’:
In summary and Rationale for this protocol – the CSPR Panel noted
- A large proportion of the serious incidents notified to the Panel are about young infants. For example, 37% of serious incident notifications in 2020 were about children less than a year old.
- There are often cases where young infants have previously presented with apparently minor injuries – with visible minor bruising – and a failure to follow established guidance, or inconsistencies within such guidance, have been highlighted as potential contributory factors to a subsequent serious incident or, ultimately, the child’s death.
This protocol has been reviewed and refreshed in line with the Child Safeguarding Practice Review Panel’s briefing and its recommendations.
Aim
To outline the pathway and actions practitioners need to follow in response to management of bruising in non-mobile infants.
Scope
All professionals at Lewisham and Greenwich NHS Trust, the London Borough of Bexley, Bromley and Lewisham who come into contact and/or work with children.
Children with disabilities
Professionals can, sometimes, have difficulty identifying safeguarding concerns in disabled children; therefore, professionals need to be aware of the increased vulnerability of this group of children so that they receive the appropriate level of protection and support.
Disability can make a child more vulnerable to abuse because:
- they may have additional communication needs
- they may not understand that what is happening to them is abuse
- they may be isolated from others
- they may be dependent on adults for all care
- their disability might be used as an explanation for an injury.
It is important to remember that children with disabilities may not be independently mobile and professionals should also seek direction from their own local guidance or national guidance.
Read the full Bruising Protocol here.
Concealed Pregnancy +
A concealed pregnancy is when a woman knows she is pregnant but does not tell any agency / professional; or when she tells another professional but conceals the fact that she is not accessing antenatal care; or when a pregnant woman tells another person or persons and they conceal the fact from all health agencies.
Where there is a strong suspicion of a concealed pregnancy it is necessary to share this, irrespective of whether consent has been given, with other agencies known to have involvement with the mother so that a fuller assessment of the available information and observations can be made.
Risks
The potential risks to a baby through the concealment of a pregnancy are difficult to predict and wide-ranging. One key implication is that there is no obstetric history or record of antenatal care prior to the birth of the baby.
Some women may present late for booking (after 24 weeks of pregnancy) and these pregnancies need to be closely monitored to assess future engagement with health professionals, particularly midwives and whether or not referral to another agency is indicated.
In a case of denied pregnancy the effects of going into labour and giving birth can be traumatic.
The reason for the concealment will be a key factor in determining the risk to the child and that reason will not be known until there has been a systemic multi-agency assessment / Pre-Birth Assessment.
Possible implications
- Concealed pregnancy can lead to a fatal outcome (for both mother and/or baby), regardless of the mothers intention. The lack of antenatal care can mean that any potential risks to mother and baby may not be detected.
- Concealment may indicate uncertainty towards the pregnancy, immature coping styles and a tendency to disassociate, all of which are likely to have a significant impact on bonding and parenting capacity.
- An unassisted delivery can be dangerous for both mother and baby, due to complications that can occur during labour and delivery.
- Lack of maternal willingness / ability to consider the baby’s health needs, or lack of emotional attachment to the child following birth.
- Where concealment is a result of alcohol or substance misuse there can be risks for the child’s health and development in utero as well as subsequently.
- There may be implications for the mother revealing a pregnancy due to fear of the reaction of family members or members of the community.
When concealment is revealed
- In some circumstances, agencies or individuals are able to anticipate the likelihood of Significant Harm with regard to an expected baby which must be addressed as early as possible to maximise time for full assessment, enabling a healthy pregnancy and supporting parents so that (where possible) they can provide safe care.
- The circumstances leading to a concealed pregnancy need to be explored individually as there may be potentially serious child protection outcomes as a result of a concealed pregnancy and a detailed interagency assessment should be undertaken.
All agencies should ensure that information about the concealment is shared with other relevant agencies, to ensure its significance is not lost and to ensure that potential future risks can be fully assessed and managed.
Pre-Birth Assessments
- Where agencies or individuals anticipate that perspective parents may need support services to care for their baby or that the baby may have suffered, or likely to suffer, significant harm, a referral to the local authority children’s social care must be made as soon as the concerns are identified. See Responding to Concerns of Abuse and Neglect Procedure, Potential risk to an unborn child.
- The importance of conducting pre-birth assessments has been highlighted by numerous research studies and case / practice reviews which have shown that children are most at risk of fatal and severe assaults in the first year of life, usually inflicted by their carer givers.
- It is important to consider the circumstances of BOTH prospective parents, not just the mother. Where possible, information should be obtained directly from each perspective parent rather than relying on a third party account.
Circumstances which might indicate an increased risk
- A child has previously sustained non-accidental injuries in the care of either parent / carer (this includes sudden, unexpected death of a child where safeguarding concerns were raised).
- Previous children have been removed from the care of the parent(s) either by a private arrangement or by a court order.
- A child in the household is the subject of a Child In Need or Child Protection Plan, or is a Looked After Child.
- Either parent is the subject of a Child in Need or Child Protection Plan, or is a Looked After Child or Care Leaver.
- The mother is a child under the age of 16 who is found to be pregnant.
- A parent or another adult in the household, or regular visitor, has been identified as posing a risk to children.
- There is concerns about the parent(s) ability to protect the baby.
- There are concerns regarding domestic violence and abuse.
- Either or both parents have mental health problems that might impact on the care of a child.
- Either or both parents have a learning disability that might impact on the care of the child.
- Either or both parents abuse substances, alcohol or drugs.
- Any other concerns exist that the baby may be at risk of Significant Harm, including a parent previously suspected of fabricating or inducing illness in a child.
- If the pregnancy is denied or concealed.
This list is not exhaustive, and professionals will need to apply their professional judgement.
Key Resources
NB: all LSCP website pages are transferable to all known languages. Please select the language from the front page. (RSS feeds G Select Language)
Modern Slavery & Child Trafficking
The Modern Day Slavery Act 2015 came into force in October 2015.
The Act
Part 1. Consolidates and clarifies the existing offences of slavery and human trafficking whilst increasing the maximum penalty for such offences. For offences of slavery, servitude and forced or compulsory labour, or for offences of human trafficking any person found guilty is liable to life imprisonment.
Part 2. Provides for two new civil preventative orders, the Slavery & Trafficking Prevention Order, and the Slavery & Trafficking Risk Order. Request of a Chief Officer of Police, Immigration Officer, or NCA can prevent foreign travel, protect potential victims, and prevent further offences.
Part 3. Provides for new maritime enforcement powers in relation to ships.
Part 4. Establishes the office of Independent Anti-Slavery Commissioner and sets out the functions of the Commissioner. To encourage good practice in investigation / victim care.
Part 5. Introduces a number of measures focussed on supporting and protecting victims, including a statutory defence for slavery or trafficking victims and special measures for witnesses in criminal proceedings. Child trafficking advocates, non prosecution of victims compelled to commit crime, presumption of under 18 until appropriate age assessment. Public body has a duty to notify suspected victim of trafficking.
Part 6. Requires certain businesses to disclose what activity they are undertaking to eliminate slavery and trafficking from their supply chains and their own business.
Part 7. Requires the Secretary of State to publish a paper on the role of the Gangmasters Licensing Authority and otherwise relates to general matters such as consequential provision and commencement.
The typology of 17 types of modern slavery offences in the UK
Labour Exploitation
|
Victims exploited for multiple purposes in isolated environments
|
Victims who are often highly vulnerable are exploited for labour in multiple ways in isolated rural locations. Victims live on offenders' property in squalid conditions, are subject to repeated abuse and are very rarely paid.
|
|
Victims work for offenders
|
Victims are forced to work directly for offenders in businesses or sites that they own or control (some offenders may be gangmasters). The main method of exploitation is not paying or illegally underpaying victims.
|
|
Victims work for someone other than offenders
|
Victims are employed in a legitimate and often low-skilled job, with legal working conditions, by an employer unrelated to the offenders. Most or all wages are taken by offenders often through control of the victims' bank accounts.
|
Domestic Servitude
|
Exploited by partner
|
Victims are forced to undertake household chores for their partner and often their partner's relatives. If married, the marriage may have been arranged or forced and the servitude often occurs alongside domestic abuse and sexual exploitation.
|
|
Exploited by relatives
|
Victims live with and exploited for household chores and childcare by family members, usually extended family. Many victims are children.
|
|
Exploiters not related to victims
|
Victims live with offenders who are often strangers. Victims are forced to undertake household chores and are mostly confined to the house.
|
Sexual Exploitation
|
Child sexual exploitation – group exploitation
|
Children are sexually exploited by groups of offenders. This is usually for personal gratification, but sometimes the exploitation involves forced sex work in fixed or changing locations and will include characteristics of types 9 and 10. Offenders frequently transport victims to different locations to abuse them.
|
|
Child sexual exploitation – single exploiter
|
Similar to type 7, often involves the grooming of children and transporting them for the purposes of sexual exploitation, although the offending is carried out by one individual.
|
|
Forced sex work in fixed location
|
Victims are trafficked and exploited in established locations set up specifically for sex work. This can include brothels or rooms in legitimate business premises (e.g. massage parlour).
|
|
Forced sex work in changing location
|
Victims are forced into sex work where the location of exploitation frequently changes. Locations include streets, clients' residence, hotels or 'pop-up' brothels in short-term rented property. Victims are frequently advertised online.
|
|
Trafficking for personal gratification
|
Victims are trafficked to residential sites controlled by offenders and sexually exploited for the offenders' own gratification. Some victims may be confined to the site for a long period of time.
|
Criminal Exploitation
|
Forced gang-related criminality
|
Victims are forced to undertake gang related criminal activities, most commonly relating to drug networks. Victims are often children who are forced by gangs to transport drugs and money to and from urban areas to suburban areas and market and coastal towns.
|
|
Forced labour in illegal activities
|
Victims are forced to provide labour to offenders for illegal purposes. The most common example is victims forced to cultivate cannabis in private residences.
|
|
Forced acquisitive crime
|
Victims are forced by offenders to carry out acquisitive crimes such as shoplifting and pickpocketing. Offenders may provide food and accommodation to victims but rarely pay them.
|
|
Forced begging
|
Victims are transported by offenders to locations to beg on the streets for money, which is then taken by offenders. Victims are often children vulnerable adults.
|
|
Trafficking for forced sham marriage
|
Traffickers transport EU national victims to the UK and sell these victims to an exploiter in a one-off transaction. Exploiters marry victims to gain immigration advantages and often sexually abuse them.
|
|
Financial fraud (including benefit fraud)
|
Victims are exploited financially; most commonly their identity documents are taken and used to claim benefits. This type often occurs alongside other types.
|
Possible Risk Indicators
A child cannot give consent to being exploited, even if they have agreed to being moved/believe they have consented, it is not "informed consent". Any child transported for exploitative reasons is considered to be a trafficking victim. All practitioners should use professional curiosity to support your ability to identify the risk factors.
- Physical symptoms, i.e. pregnant, STI's, sexual or physical assault, poor dental health. May show signs of physical or psychological abuse, look malnourished or unkempt, or appear withdrawn.
- Victims may rarely be able to travel on their own, seem under the control or influence of others, rarely interact, or appear unfamiliar with their neighborhood or where they work.
- Involved in criminal activity, i.e. cannabis factory, begging, pick pocketing.
- Foreign national child. Brought or moved from another country. Has false documentation, or no passport or ID.
- With an adult, but unclear what the relationship is.
- Concerns about the relationship between the parent and child.
- With an adult who speaks for the child.
- Orphaned or separated from family or main carers.
- Possesses money or goods not accounted for.
- Has not been registered with a GP.
- May or may not be enrolled at a school.
- Homeless child.
- An unrelated or new child discovered at an address.
- Found in a brothel or sauna.
- May be working in catering, nail bars, caring for children, cleaning etc.
- Links to adult(s) with offending history.
- Missing child. There is a strong possibility the child will be re-trafficked within 24-48 hours of being placed in care.
Procedure in Lewisham
Child Trafficking and Slavery are Child Protection issues and the normal procedures apply. You can make a referral to the Multi-Agency Safeguarding Hub by telephone 020 8314 6660 or by email mashagency@lewisham.gov.uk or complete a MASH Referral Form.
Useful Contacts
- Athena Service lewishamvawg@refuge.org.uk 0800 112 4052
- NSPCC Child Trafficking Advice Centre (CTAC): 0808 800 5000 ctac@nspcc.org.uk
- UK Human Trafficking Centre: 0844 778 2406, UKHTC@nca.x.gsi.gov.uk
- Refugee Council Advice Line: 020 7346 1134
- ECPAT UK: 020 7233 9887 ecpat.org.uk
- Coram Legal Centre: www.childrenslegalcentre.com
- Children and Families Across Boarders (CFAB) 020 7735 8941 cfab.uk.net
- Foreign & Commonwealth Office: 020 7008 1500
- CEOP 020 7238 2320/2307 ceop.gov.uk
- Home Office http://www.crimereduction.homeoffice.gov.uk/toolkits/tp01.htm
Additional Guidance
Resources & Publications
A typology of modern slavery offences in the UK October 2017
Home Secretary Amber Rudd announces new measures to improve identification and support for victims of modern slavery. October 2017
Home Office Resources
ACPO Guidance
CPS
Trafficking Toolkit
Human Trafficking Strategy
London Safeguarding Children Board - Trafficked Children toolkit and guidance
Safeguarding Children who may have been trafficked (2011) DfE
Home Office UK Border Code of Practice for Keeping Children Safe from Harm
Multi-Agency Child Exploitation (MACE) Strategy & Resources
It is recognised that procedures and systems developed to safeguard children and young people from risks within the home environment or family can be less effective in addressing extra familial harm. In the last decade Local Authorities began to introduce MACE (multiagency sexual exploitation panels) and many police forces introduced Child Sexual Exploitation (CSE) Teams .
The MACE panel’s focused on CSE and were introduced in response to learning form a number of serious case reviews concerning children that had suffered significant harm due to being sexually exploited. As adolescent safeguarding practice developed over the last decade, professionals, agencies and the public developed a greater awareness of how extra familiar harm impacted on children and young people. The multi-faceted nature of adolescent risk became apparent to Local Authorities and safeguarding partners, in addition to child sexual exploitation it was recognised that children & young people were also at risk of criminal exploitation, youth violence and online exploitation. Agencies began to learn more about specific forms of exploitation such as county lines.
In response to the changing nature of extra familial harm, many Local Authorities across the country began to expand the remit of their MACE panels to cover all forms of child criminal exportation. This development happened at the local level, while there was a common theme of including all forms of extra familial harm, each Local Authority across London developed slightly different processes and procedures, for example Lewisham introduced the Concern Hub in 2019.
There was an expansion of MACE style panels across London following a review in 2020, London wide guidance (2021) was issued and recommended that Local Authorities set up MACE (multi-agency child exploitation) panels and structures. The London guidance recognises that Local Authorities need to respond to local challenges and issues, however provides some common guidance and structure. This will provide some cross Borough consistency and is particularly welcomed by agencies who operate across a number of London Boroughs.
New MACE arrangement for Lewisham
In response to London guidance, the Lewisham partnership reviewed our local arrangements (Concern Hub). In January 2022 we started to transition from the Concern Hub model to a MACE structure based on the new London guidance. In order to ensure that we develop a MACE structure which met Lewisham’s specific needs the partnership has taken an agile approach to the development and implementation Lewisham’s MACE.
The Lewisham MACE provides a strategic, tactical and operational response to extra familial harm to children and young people across Lewisham. The definition of extra familial the purpose MACE includes sexual exploitation, criminal exploitation, county lines, serious youth violence and harmful sexual behaviour. The strategic approach to exploitation in Lewisham encompasses 4 key strands Pursue , Prevent, Protect and Restore. In developing a Lewisham MACE, the partnership has taken into account some of the unique and innovative aspects that the Concern Hub embodied. The Lewisham MACE considered young people up to the age of 25 and maintains a strong focus on community safety and addressing serious youth violence.
MACE Structure
The partnership have developed a 3 tiered MACE structure, to support partnership working across key agencies to address the multifaceted nature of extra familial harm to children and young people within the local context.
- Pre—MACE, This is a bi-weekly operational meeting co-chaired by police and children social care. The purpose is to review referrals, ensure appropriate safeguarding with the MACE risk rating. The pre-mace identifies high risk cases or thematic issues to be escalated to the monthly MACE .
- MACE (tactical) this is a monthly panel including key safeguarding partners and co-chaired by a Senior Police Officer and a Senior Children Social Care Manager. The panel review high risk cases escalated by pre-mace, to ensure that all agencies are working effectively together and using all powers and resources at their disposal to ensure that the child or young person is safeguarded. The panel review exploitation related data from a number of sources and thematic issues raised by partners to ensure there is an appropriate multiagency tactical response.
- MACE Strategic. The strategic panel is made up of senior managers from across the partnership and is chaired by the police. The strategic mace is responsible for the implementation of the Child Exploitation Strategy and Action Plan. The Strategic MACE reports directly to the LSCP Executive.
The MACE does not in any way replace established statutory safeguarding procedures and professional should always follow up the established safeguarding pathway. If any professional, individual or family member is concerned for the welfare or safety of a child they should make a MASH referral or in the case of the child with an allocated social worker contact the social worker directly. If it is believed that the child is in imminent risk of harm, the advice is to contact emergency services on 999 before contacting children social care.
Referral pathway.
It is encouraged that Social Work Teams convey a Strategy Meeting prior to referring to pre-mace, this is to ensure that all immediate safeguarding actions are taken and information is shared with key agencies. It is the responsibility of the Social Work Team to make a pre-mace referral if they believe the child or young person they are working with is at risk of sexual exploitation, criminal exploitation, serious youth violence or harmful sexualised behaviour. All pre-mace referrals concerning children should be made by the allocated social worker or lead professional.
In the case of young adults aged 18 to 25, if they are Care Leavers it is the responsibility of the personal advisor, to complete a pre-mace referral. If the young person aged 18 to 25 is not a care leaver any can make a referral directly into the young adults pre-mace.
Lewisham Child Exploitation Strategy
Appendix A Forms of Child Exploitation
Appendix B Child Exploitation Key Indicators
Appendix C Best Practice - Safeguarding & Child Exploitation Processes
Appendix D Local and National Child Exploitation Resources
Appendix E MACE Referral Pathway
Appendix F MACE Referral Form
Appendix G Strategic Business Plan
Page under development
Neglect
There are many factors that influence and shape the development of a child. Some are within the child, such as genetic factors, and others are from external sources such as physical, psychological and family influences, as well as the wider neighbourhood and cultural aspects.
Neglect is therefore often complex and not always immediately recognised. The impact will vary according to type, severity and length of time, making it difficult for those working with children and families to manage. Professional uncertainty, differences of opinion or undue optimism regarding levels of need and the criteria for significant harm can lead to long term exposure which substantially increase the risk to children.
Neglect of children remains one of the Lewisham Safeguarding Children Partnership (LSCP) key priorities. This strategy has been developed with multi-agency partners to set out Lewisham’s approach to PREVENT RESPOND to AND REDUCE child neglect in Lewisham.
This strategy should be viewed alongside the following key strategies, policies and procedures and government guidance in relation to neglect:
The Definition
Working Together to Safeguard Children (2023) describes neglect as:
The persistent failure to meet a child’s basic physical and/or psychological needs, likely to result in the serious impairment of the child’s health or development. Neglect may occur during pregnancy as a result of maternal substance abuse. Once a child is born, neglect may involve a parent or carer failing to:
- provide adequate food, clothing and shelter (including exclusion from home or abandonment)
- protect a child from physical and emotional harm or danger
- ensure adequate supervision (including the use of inadequate care-givers)
- ensure access to appropriate medical care or treatment
It may also include neglect of, or unresponsiveness to, a child’s basic emotional needs.’
Why is this important in Lewisham?
Neglect is the most common reason for a child to be the subject of a child protection plan in the UK. In Lewisham, neglect is one of the highest risk factor indicators.
What do professionals need to do?
Although you may be worried about a child, it’s not always easy for professionals to identify neglect. There’s often no single sign or incident that a child or family need help. It is more likely that there will be a series of concerns over a period of time that, taken together, demonstrate the child is at risk. If you think a child may be experiencing neglect, don’t wait:
- Gather all relevant information about the child, including the parenting capacity and family and environmental factors in order to form a professional judgment on strengths, risks and harmful factors
- Use professional curiosity to understand the child and families lived experiences.
- Use our newly developed Signs of Safety Neglect Screening Tool to help you identify concerns about whether the child’s needs are being neglected. This will assist with the early identification of neglect or in coordinating support for families in need of additional help. The checklist can also be used to track improvements, deterioration, or ‘drift’
- Regularly review progress using the screening tool below and update the multi-agency plan accordingly.
- Where there are concerns about a child’s needs or their needs are unclear, a Common Assessment (CAF) should be considered in line with LSCP Family Help Continuum of Need 2024-2025 (final)
Signs of Safety Neglect Screening Tool
Signs of Safety Neglect Screening Tool Guidance Framework
Introduction to the Signs of Safety Neglect Screening Tool video - Alex Campbell, Lewisham Workforce Development Group
LSCP Multi-Agency Neglect Strategy 2023-2026
LSCP Neglect Strategic Action Plan 2023-2026
On-line Safety
The internet is a great way for children and young people to connect with others and learn new things. As interactions between people are increasingly taking place on-line it is essential that we safeguard children as robustly in the virtual world as we do in the real one. We can do this through:
- Promoting safe on-line behaviour to children, young people and their families
- Taking children, young people and their families’ on-line actions and networks into account when providing support
Children, young people and their families go online for a variety of reasons, including:
- To search for information or content on search engines
- Share images and watch videos through websites or mobile apps
- Use social networking websites
- Write or reply to messages on forums and message boards
- Play games along or with others through websites, apps or games consoles
- Chat with other people through on-line, games, messenger apps, games consoles, webcams, social network, and other instant communication tools
- Find new friends and partners
There are lots of benefits in going on-line, and also some risks. These include:
- Exposure to and sharing of explicit material (including sexting)
- Grooming
- Radicalisation
- Exploitation
- Identity theft
- Cyber-bullying
- Cyber-hacking
It’s important that as professionals you are confident in talking with children, young people and their families about their on-line choices and interactions. This includes tablets, lap-tops, phones etc, for example:
- Personal information shared on-line: checking privacy settings, sharing contact details, geotagging
- Images shared and online communication: on-line support networks, inappropriate images (e.g. sexting), online bullying or harassment
- On-line relationships: safe online friendships, meeting up with on-line friends or potential partners
LSCP E-Safety Guidance - June 2017
Advice and resources
CEOP Thinkuknow provides advice for parents and carers, children and young people, and those that work with them.
NSPCC Online Safety has further advice and tools.
Child Exploitation & Online Protection (CEOP)
CEOP is there to support young people, parents and carers while surfing online, and offers help and advice on topics such as:
- cyberbullying
- hacking
- harmful content
It also enables people to immediately report anything on-line which they find concerning, such as harmful or inappropriate content, or possible grooming behaviour.
For more information, or to report concerns, simply click on the CEOP Icon

Physical Abuse of Children & Young People
 Dfe campaign website
Dfe campaign website
Definition
To use physical force that results in an injury, physical pain, or impairment. This may include hitting, beating, pushing, shoving, throwing, shaking, slapping that leaves a mark, kicking, pinching, punching, suffocation, pulling hair out, burning, or striking with an object, hands, or feet. Being made to swallow something that hurts or causes illness, i.e. forcing the taking of medicine when a child is not ill - Also known as Fabricated Induced Illness. Being made to sit or stand in uncomfortable positions or locked in small spaces.
What is the Law?
In the UK it is unlawful for a parent or carer to smack their child, except where this amounts to "reasonable punishment". This defence is laid down in Section 58 of the Children Act 2004.
Whether a smack amounts to reasonable punishment will depend on the circumstances of each case, taking into consideration factors like the age of the child and the nature of the smack. There are strict guidelines covering the use of reasonable punishment and the Director of Public Prosecutions for England and Wales has produced a charging standard of categorisation in order to assist prosecutors to determine the appropriate charging offence. It will not be possible for a parent/carer to rely on this defence if the physical punishment amounts to wounding, actual bodily harm, grievous bodily harm or child cruelty.
Cultural tradition or adults perceived ideas of parental rights to use physical force as a way of discipline must not stand in the way of protecting a child from physical abuse.
Current Statistics
The NSPCC report that although exact numbers of physical abuse are not known, it is estimated that 1 in 4 children have been physically abused. Disabled children are 3 times more likely to be abused than non-disabled children. In 2016-17 over 6,800 children were identified as needing protection from physical abuse, with 11,000 children contacting help lines for support - 22% of those cases were referred to the Police. In 2017 7,000 ChildLine counselling sessions were about physical abuse.
Signs & Symptoms of Physical Abuse
The child may have:-
- Regular bruising anywhere on the body, including defensive bruises to the arms or bruises shaped like an instrument or hand.
- Bruises with dots of blood under the skin.
- A bruised scalp and swollen eyes from the hair being pulled violently.
- Broken bones or fractures.
- Burns or scalds, including small round burns from a cigarette or sharp edged burns.
- Bite marks usually round or oval shaped.
You may notice:-
- The child may regularly avoid taking part in sports activities or reluctant to get changed in front of others.
- Becomes withdrawn, flinches, is anxious, clingy, or suddenly behaves differently.
- May be depressed, or develop obsessive behaviour.
- Have problems sleeping, frequent nightmares, bed wetting, or soils clothes.
- There may be changes in the child's eating habits or the child may develop an eating disorder.
- The child may bully or hurt other children and become aggressive.
- They may develop risky behaviours, i.e. taking drugs, alcohol, self-harm, or have thoughts about suicide.
- The child may regularly miss nursery or school. Children have accidents, trips and falls. However, if a child regularly has injuries, you notice a pattern, or the explanation does not match the injury you should use professional curiosity and investigate to ascertain if a child is being physically abused and make a referral to Children's Social Care. Adults who physically abuse children may have emotional or behavioural problems such as difficulty controlling their anger. They may have family or relationship problems or have experienced abuse as a child. They may have parenting difficulties including unrealistic expectations of children, they may not have an understanding of a child’s needs, or have no idea how to respond to a child.
Effects of Shaking a Baby
If a baby is shaken or thrown, they may suffer non-accidental head injuries. Shaking a baby can cause fractures, internal injuries, long-term disabilities and even death.
The most serious consequence of a non-accidental head injury (NAHI) is a brain injury which can lead to learning problems, seizures, hearing and speech impairment, visual impairment or blindness, behaviour problems or changes in personality, severe brain damage, long-term disability, or even death. Babies may suffer other injuries from the abuse such as broken bones or fractures.
Good Advice to Parents/Carers on How to Discipline Without Smacking
-
- Provide love and emotional warmth as much as possible.
- Have clear simple rules, boundaries and explain actions to the child so they understand what is expected of them.
- Be a good role model.
- Praise good behaviour so it will increase, and ignore behaviour which is not to be repeated.
- Criticise behaviours and not the child.
- Reward good behaviour with hugs and kisses.
- Distract young children or use humour.
- Young children often respond well to a wall chart marking good behaviour, setting targets and agree on a small reward.
- Allow children some control, make joint decisions and give choices.
- If punishment is necessary, remove privileges, or take time out.
- Have a strategy in place and think about your reactions before feelings escalate.
- Seek support from the local Children's Centre or Parent Support Group.
Long Term Effects of Physical Abuse
The long term impact of child abuse is far reaching, some studies indicate that without the right support, the effects of childhood abuse can last a lifetime. These effects can be characterised by frequent crisis, failed relationships or difficulty maintaining family relationships, chaotic lifestyles, and are highly likely to have a psychiatric disorder such as depression, anxiety, personality disorders, or eating disorders.
Procedure in Lewisham
If you become aware or suspect a child is being physically abused, has an injury that is not consistent with the explanation provided, or a disclosure is made by a child, you must immediately contact the MASH Team on:-
Telephone Number: 020 8314 6660
Email: mashagency@lewisham.gov.uk
If a child is in immediate danger call 999.
You have a duty of care to seek medical attention for the child if necessary.
Children’s Centres
Children’s Centres are able to offer a range of support for parent(s) who may be struggling to cope. You can contact your local Children’s Centre for any one of the services below:-
- Family and parenting support, including family learning and parenting courses.
- Advice on early-years education and childcare, including eligibility for free education and childcare for 2–4-year-olds.
- Child and family health services, including baby hubs and breastfeeding support.
- Volunteering and employment support, including links to Jobcentre Plus.
- Information and advice about children’s services and schools.
- Drop-in services covering health, education and a range of other areas such as debt management, counselling and SENDIASS.
Useful Links
- DfE, Together we can tackle child abuse
- NSPCC
Prevent Strategy
What is CONTEST and the Prevent Strategy?
The Prevent Strategy is one of the key elements of CONTEST, the Government's counter- terrorism strategy and it aims to stop people from being drawn into terrorist-related activity. Prevent has strong links to safeguarding because vulnerable children and adults can be susceptible to radicalisation and recruitment into violent extremist and terrorist organisations.
CONTEST has four strands:
- Protect: Strengthen our protection against terrorist attack.
- Prepare: Mitigate the impact of an attack.
- Pursue: Stop a terrorist attack.
- Prevent: Stop people from becoming terrorists or supporting terrorism by:
-
- responding to the ideological challenge of terrorism and the threat we face from those who promote it,
- preventing people from being drawn into terrorism and ensuring that they are given appropriate advice and support,
- working with sectors and institutions where there are risks of radicalisation that we need to address.
What does the Prevent Duty mean for Statutory Organisations in Lewisham?
Since 2015, statutory agencies have a duty under the Counter Terrorism & Security Act "to have due regard to the need to prevent people from being drawn into terrorism". This means that local authorities should:
- Establish strategic and operational links with other specified authorities,
- Facilitate the assessment of risk for specified authorities, including providing advice and sharing threat assessments based on the Counter Terrorism Local Profiles (CTLP),
- Understand the full range of bodies affected by the new duties, and ensure they understand their responsibilities,
- Embed Prevent into commissioning, procurement, and grant funding processes,
- Embed Prevent into Safeguarding Policies and ensure all providers are signed up to local Safeguarding arrangements.
Lewisham Prevent Service
LBL Prevent are available to assist agencies in complying with their Counter Terrorism Act duties. The support offer includes:
- The sharing of training opportunities to upskill frontline staff and those with additional safeguarding responsibilities.
- Management briefings regarding Prevent Duty compliance,
- Coordination of strategic and operational groups,
- The provision of Prevent-related resources and dissemination of relevant information.
Safeguarding children and young people against radicalisation and extremism
There have been several cases where extremist groups or individuals have attempted to radicalise vulnerable children. This can include justifying political, religious, sexist, or racist violence, or to steer individuals towards an ideology of extremism and intolerance. A young person might be groomed and radicalised into carrying out acts of violence and cause significant harm to others.
There are several ways in which children and young people can be at risk of radicalisation
- They can be groomed either online or in person by people seeking to draw them into extremist activity.
- Young people can be radicalised online via peer networks, social media, or online chat platforms.
- Grooming of a young person can also be carried out by those who hold harmful, extremist beliefs, including family members or friends who have an influence over the young persons life.
- Young people can be exposed to violent, anti-social, extremist imagery and narratives which can lead to normalising intolerance of others and extremist ideology.
As with other forms of safeguarding strategies, early intervention is essential. All agencies working with children and young people, along with families and communities can play a vital role in ensuring young people and their communities are safe from the threat of radicalisation, extremist ideologies and terrorism.
If you are concerned that a child, young person and/or parents/carers or other family members may hold extremist views or are at risk of being radicalised, it is important to ensure that they receive support to protect them from being drawn into terrorism.
Making a Referral
If you are worried about a child or a young person you should follow your own organisation’s child protection procedures without delay.
If a child is in immediate risk call 999.
To make a Prevent referral, practitioners should complete a Prevent Referral Form and email it to preventreferrals@met.pnn.police.uk.
Ensure that Lewisham’s MASH team (mashagency@lewisham.gov.uk) and prevent@lewisham.gov.uk are copied in to this email.
If you have any questions regarding Prevent in Lewisham you can contact the Prevent team by emailing: prevent@lewisham.gov.uk
The Channel Programme
Channel is a voluntary and confidential support programme which safeguards people who have been identified as vulnerable to being drawn into terrorism.
This multi-agency programme involves partners from the local authority, the police, education sector, health providers and other groups.
Channel offers various types of support that will address educational, vocational, mental health and other vulnerabilities.
It is not a criminal sanction and it will not affect a person’s criminal record.
What happens after a Prevent referral is made
When someone makes a referral, lots of agencies work together to offer support where it is necessary and proportionate to do so. This involves several steps:
The police carefully assess all referrals to see if they are suitable for Channel or whether a different type of support is more appropriate, such as mental health support.
If suitable, the referral is discussed with all relevant partners at a meeting called a Channel panel to decide if an intervention is necessary. The individual who has been referred to Prevent is informed and must give their consent (or via a parent or guardian if they are under the age of 18) before an intervention can take place.
If Channel intervention is required, the panel works with local partners to develop an appropriate tailored support package.
The support package is monitored closely and reviewed regularly by the Channel panel.
Training
Prevent Awareness Course (30-40 minutes)
This e-learning package is provided by the Home Office and is intended for frontline professionals working in a safeguarding role. It covers how Prevent is relevant to your role, as well as spotting the signs of radicalisation and recognising some of the emotions and behaviours that might make someone susceptible to radicalisation.
Participants receive a certificate of completion, which can be used to demonstrate compliance.
It is recommended that all frontline professionals refresh their knowledge with full training every two years.
Access the full course here: https://www.support-people-susceptible-to-radicalisation.service.gov.uk/portal#awareness-course
For professionals who have already completed Prevent training, there is a short refresher course, which is recommended is completed annually: https://www.support-people-susceptible-to-radicalisation.service.gov.uk/portal#refresher-awareness-course
Prevent Referrals Course (30-40 minutes)
This course is primarily designed for professionals with a designated safeguarding role and covers how to make a well-informed Prevent referral. It includes the key principles of making a Prevent referral, how to identify valid causes for concern and what information to gather.
Access the course here: https://www.support-people-susceptible-to-radicalisation.service.gov.uk/portal#referrals-course
Channel Awareness (50-60 minutes)
This course is for anyone who may be asked to sit on a Channel panel. This might the Designated Safeguarding Lead at a school where a child has been referred, or an assigned social worker.
It covers what a Channel panel is and how it functions, and prepares you for attending.
Access the course here: https://www.support-people-susceptible-to-radicalisation.service.gov.uk/portal#awareness-course
Additional Training Opportunities
Professionals working in Lewisham Schools can find out more about additional training opportunities and support offered through the Department for Education here: Prevent Resources | Lewisham Services for Schools
Occasionally, the Home Office share additional training workshops which dive deeper into different elements of Prevent. These are circulated by the LSCP Business Unit. To sign up to the mailing list please email safeguardingpartnership@lewisham.gov.uk.
Lewisham Council is unable to provide Prevent training directly to settings and agencies.
Public Advice
- If you wish to advise members of the public about extremism and radicalisation, you can signpost them to Act Early, the UK’s counter-extremism support line
- Act Early also have a range of public-facing resources, including posters and leaflets, that you can download for your setting here: Act Early Resources
- If you see or hear anything that could be terrorist-related, trust your instincts and call the Anti-Terrorist Hotline on 0800 789 321.
- If you think you have seen a person acting suspiciously, or if you see a vehicle, unattended package or bag which might be an immediate threat, move away and call 999.
- If you are involved in an incident follow police advice to: 'RUN, HIDE AND TELL'
- Download the citizenAID App, which provides safety and medical advice from Google Play, Apple App or the Windows Store, for free.
Guidance
Resources for parents and practitioners
General online safety guidance
Private Fostering Arrangements


What is Private Fostering?
Private fostering is when children and young people under the age of 16 years or under 18 if they are disabled, are cared for on a full time basis by a person who is not their parent, who does not have parental responsibility or who is not a close relative for 28 days or more. A relative is defined in the Children Act 1989 as a grandparent, uncle or aunt (whether by full-blood, half-blood or by marriage or civil partnership), sibling or step-parent.
Who are not close relatives?
Family friends, cousins, great aunts and great uncles do not count as close relatives (As defined in the Children Act 1989). There are many circumstances in which an unmarried partner becomes the carer for a child. A parent’s unmarried partner is not a step-parent in this context. It is a common misunderstanding and parents/carers are often unaware of the legal requirements to notify the local authority of a private fostering arrangement.
Caring for someone else's child is not private fostering when the arrangement is made by the Local Authority, or when the person looking after a child is an approved foster carer.
What are examples of private fostering arrangements?
The fostering arrangement is made privately between the parent and the person looking after the child or young person.
Lots of different situations count as private fostering, including:
- A child or young person whose parent (s) cannot look after them because of illness, work or study long or antisocial hours;
- A child or young person are living with a friend’s family because of parental separation, divorce or arguments at home
- A child or young person are living with their partner’s family;
- A child from abroad sent to stay with another family in the UK for education or heath care by their birth parents;
- An asylum seeking or refugee child;
- Children who may have been trafficked into the country
- A child or young person who, having broken ties with their family, is staying with friends or other non-relatives usually on a short term basis;
- A language student living with a host family; or
- A child or young person staying with a family while attending a school away from home.
Who needs to tell us about a private fostering arrangement?
You should encourage parents/carers to notify Lewisham Multi-agency Safeguarding Hub (MASH) Team. If you feel that we have not been made aware by parents/carers, then you should notify Lewisham MASH Team:
Email: mashagency@lewisham.gov.uk
Phone: 020 8314 6660
What happens next?
- When the private fostering team have this information a social worker will contact the parents and carers to arrange a visit to explain the legal requirements and procedures for private fostering.
- The Private Fostering Social Worker must visit the child and private foster family within 7 days of being notified.
- The Private Fostering Social Worker will do safeguarding checks on the host family and complete a private fostering assessment in regards to the carers’ suitability to look after that child within 42 days, this is not a Single Assessment.
- If the private fostering assessment is suitable and proves to promote child’s welfare, subsequent visits must be carried out in the 1st year of the arrangement at intervals of 6 weeks, in the 2nd & subsequent years, visits must take place every 12 weeks and more often if required not necessarily with parental consent.
- Private fostering assessments and visit reports must be completed after every visit & authorised/signed off at a managerial level however this remains a private arrangement.
Important things to note
- Parents retain Parental Responsibility (PR) and their consent will be needed for everything done for that child including medical appointments, haircuts etc. If Early Help is deemed to be appropriate, parental consent will be needed for this. The Private Fostering Social Worker may liaise with parents in some circumstances in order to help facilitate this type of consent being given.
- If Social Care say that it is not suitable for that child to return to their family home at any stage, then this is not a Private Fostering case and Children’s Social Care involvement will be necessary.
- If a child already has a Social Worker and is open to Lewisham Children’s social care, you will need to inform their Social Worker of the child’s new living arrangements. The Social Worker will then notify the Private Fostering team so they can assess the private foster family, the child’s allocated Social Worker will retain full case responsibility.
- If the arrangements are unsuitable, it will be necessary to consult with the Service Manager who may seek legal advice, with a view to considering initiating prohibiting procedures. Parents will be advised to make alternative arrangements for their child and a further referral made to MASH if necessary.
Where can I find more information?
Private Fostering social worker: Anna Luckock
Tel: 07392 286612
Email: SG.support@lewisham.gov.uk
Lewisham council website: https://lewisham.gov.uk/myservices/socialcare/children/fostering/private-fostering
Lewisham Multi-agency safeguarding hub (MASH) Team
Email: mashagency@lewisham.gov.uk
Telephone: 020 8314 6660
Coram baaf: https://corambaaf.org.uk/practice-areas/kinship-care/information-kinship-carers/what-private-fostering
Practitioners should, in particular, be alert to the potential need for early help for a child who are privately fostered – Working Together to Safeguard Children (2018, p13)
Questions to consider asking to help you identify a child who is Privately Fostered
- Do you suspect that a child may be privately fostered?
- Has the child mentioned that they are no longer living at home / living with someone else?
- Is the child accompanied to school/nursery/clinic by someone other than a parent/recognised carer?
- Is the carer vague about the child’s routines/needs?
- Has a patient turned up at the GP surgery with a new child/ series of different children?
- Has a child in class at school disappeared?
- Is there anything unclear on files/records about the child’s living arrangements?
- Is the child under the age of 16 (or 18 if disabled)?
- Is the child living with someone other than a parent, someone with parental responsibility or a close relative (A relative is defined in the Children Act 1989 as a grandparent, uncle or aunt (whether by full-blood, half-blood or by marriage or civil partnership), sibling or step-parent.)
- Do you know what the child’s living arrangements are (who with, for what purpose)?
- Is it clear who the child is living with, and what relation the person is to the child?
- Has the child been living, or is likely to live, away from home for more than 28 days?
- Has the child come from overseas? Do you know the reason for the child’s entrance to the UK?
- Is the child in the UK for the purpose of education?
- Is the child an unaccompanied asylum seeker?
- Do you think that the child may have been trafficked?
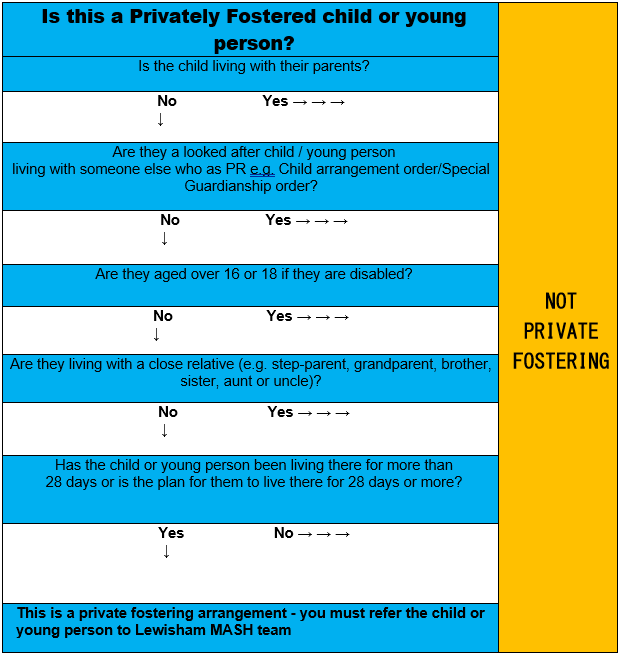
Additional Information for Professionals:
How is private fostering different to foster care?
Foster care
Foster care is when children are placed with foster carers through arrangements made by Local Authorities. All foster carers have been approved by a Local Authority or independent fostering service provider prior to caring for any children.
Private fostering
Private fostering arrangements are made without the involvement of the Local Authority – they are usually made by the parents of the child or another adult or on some occasions by young people themselves. Although the Local Authority is not involved in making these arrangements, it is important that they are notified about them.
Why should a Local Authority be made aware of private fostering arrangements?
Safeguarding the child
Privately fostering a child is always a big responsibility, and the Local Authority has a duty to oversee the arrangements to promote the welfare of the child and to ensure they are protected. It is important that the carer has a good understanding of the child's needs.
Providing support
Taking on the care of someone else's child is not often straightforward. Misunderstandings and conflicts can easily arise, even between friends. Living away from their parents for any length of time can present challenges to children and their carers, and the Local Authority can support them both.
Further information can be found from the Lewisham council website: https://lewisham.gov.uk/myservices/socialcare/children/fostering/private-fosteringwebsite.
Coram BAAF: https://corambaaf.org.uk/practice-areas/kinship-care/information-kinship-carers/what-private-fostering?gclid=EAIaIQobChMI0MG26pmM-AIVgQsGAB2ZsATwEAAYAiAAEgJuJvD_BwE
Professional Curiosity & Challenge
Nurturing professional curiosity and challenge are a fundamental aspect of working together to keep children and young people safe.
In this resource we will raise awareness of the need for respectful uncertainty; help practitioners spot the signs of when a parent or carer may be using disguised compliance; and advise where and how to access help and services.
What is professional curiosity?
Professional curiosity is the capacity and communication skill to explore and understand what is happening within a family rather than making assumptions or accepting things at face value.
This has been described at the need for practitioners to practice ‘respectful uncertainty’ – applying critical evaluation to any information they receive and maintaining an open mind. In safeguarding the term ‘safe uncertainty’ is used to describe an approach which is focused on safety but that takes into account changing information, different perspectives and acknowledges that certainty may not be achievable.
Professional curiosity can require practitioners to think ‘outside the box’, beyond their usual professional role, and consider families’ circumstances holistically.
Professional curiosity and a real willingness to engage with children, adults and their families or carers are vital to promoting safety and stability for everyone.
Much has been written about the importance of curiosity during home visits and the need for authentic, close relationships of the kind where we see, hear and touch the truth of their experience of ‘daily life’ and are able to act on it and to achieve similar closeness with parents or carers.
Practitioners will often come into contact with a child, young person, adult or their family when they are in crisis or vulnerable to harm. These interactions present crucial opportunities for protection. Responding to these opportunities requires the ability to recognise (or see the signs of) vulnerabilities and potential or actual risks of harm, maintaining an open stance of professional curiosity (or enquiring deeper), and understanding one’s own responsibility and knowing how to take action.
Children in particular, but also some adults, rarely disclose abuse and neglect directly to practitioners and, if they do, it will often be through unusual behaviour or comments. This makes identifying abuse and neglect difficult for professionals across agencies. We know that it is better to help as early as possible, before issues get worse. That means that all agencies and practitioners need to work together – the first step is to be professionally curious.
Curious professionals will spend time engaging with families on visits. They will know that talk, play and touch can all be important to observe and consider. Do not presume you know what is happening in the family home – ask questions and seek clarity if you are not certain. Do not be afraid to ask questions of families, and do so in an open way so they know that you are asking to keep the child or adult safe, not to judge or criticise. Be open to the unexpected, and incorporate information that does not support your initial assumptions into your assessment of what life is like for the child or adult in the family.
Thinking the unthinkable
Safeguarding is everyone’s responsibility, and where practitioners are concerned each and every agency has a role to play in safeguarding and protecting children.
The following factors highlight the need for all of us to strive to improve professional curiosity and professional courage:
- the views and feelings of children and some adults are actually very difficult to ascertain
- practitioners do not always listen to adults who tried to speak on behalf of a child or another adult and who may have important information to contribute
- parents or carers can easily prevent practitioners from seeing and listening to a child or another adult
- practitioners can be fooled with stories we want to believe are true
- effective multi-agency work needs to be coordinated
- challenging parents or carers (and colleagues) requires expertise, confidence, time and a considerable amount of emotional energy.
What is disguised compliance?
Professional curiosity or respectful uncertainty is needed when working with families who are displaying disguised compliance. Disguised compliance involves parents or carers giving the appearance of co-operating with agencies to avoid raising suspicions and allay concerns.
There is a continuum of behaviours from parents or carers on a sliding scale, with full co-operation at end of the scale, and planned and effective resistance at the other. Showing your best side or ‘saving face’ may be viewed as ‘normal’ behaviour and therefore we can expect a degree of disguised compliance in all families; but at its worst superficial cooperation may be to conceal deliberate abuse; and many case reviews highlight that professionals can sometimes delay or avoid interventions due to parental disguised compliance.
The following principles will help front line practitioners deal with disguised compliance more effectively:
- focus on the needs, voice and ‘lived experience’ of the child, young person or adult
- avoid being encouraged to focus to extensively on the needs and presentation of the adults or carers – whether aggressive argumentative or apparently compliant
- think carefully about the ‘engagement’ of the adult or carers and the impact of this behaviour on the practitioners view of risk
- focus on change in the family dynamic and the impact this will have on the life and well-being of the child or adult – this is a more reliable measure than the agreement of adults or carers in the professionals plan
- there is some evidence that an empathetic approach by professionals may result in an increased level of trust and a more open family response leading to greater disclosure by adults and children
- practitioners need to build close partnership style relationships with families whilst being constantly aware of the child needs and the degree to which they are met
- there is no magic way of spotting disguised compliance other than the discrepancy between an adult or carer’s accounts and observations of the needs and accounts of the child. The latter must always take precedent.
Communication - the key to good multi-agency working
Top tips:
- speak to other practitioners on a regular basis – don’t wait for meetings
- when assessing and managing a case, input from two, three or four sources is better than one
- sometimes the most important relationship to trust is yourself – if you feel there is a risk that is not being managed and no one is hearing you what do you do, how do you escalate this?
- try to be flexible with meetings to fit around all involved practitioners availability
- don’t use jargon – talk to colleagues and families using language they understand and relate to
- include families in decisions about their own lives
- be mindful of personal optimistic bias (wishful thinking) when reviewing the families’ progress
- make sure care plans are multi-agency and SMART
- self-assessments tools can promote honest discussion
- team managers should attend training for providing effective supervision and reflective practice in managing safeguarding
- use quality assurance and audit framework such as quality standards to review case records to support good practice that keeps children safe and aids staff continuous professional development (CPD).
Information sharing:
- to support good communication, a formal information sharing arrangement should be in place between all agencies with the purpose and content about requesting and sharing information explicitly agreed
- fears about jeopardising the relationship with the family should not be a barrier to the sharing of information
- principles from "the seven golden rules for information sharing" should be followed
- information should be shared in a timely manner and the family included where it does not increase risk
- all involved agencies should be given ample notice when invited to case review meetings to enable them to provide reports and feedback to contribute to ongoing assessment and review of family progress
- a group of practitioners should maintain contact with each other and make the times of meetings flexible to enable optimal attendance of practitioners.
Difficult conversations with parents and carers
Open discussion with parents and carers when there are welfare concerns about a child often provokes anxiety in practitioners. Professional challenge is part of good child protection practice.
To increase practitioners’ confidence we have published a "How to have difficult conversations with parents/carers" guide.
The information in this guide is not exhaustive and it should be used as a reference tool alongside practitioners own safeguarding practices and in conjunction with appropriate supervision.
Four factors to consider when preparing for a difficult conversation with a parent or carer are:
- Principles – that underpin safeguarding children
- Planning – how to plan or be prepared
- The conversation – things to consider when having a conversation
- Examples – open questions and suggestions.
Professional challenge - having different perspectives
Differences of opinion, concerns and issues can arise for practitioners at work and it is important they are resolved as effectively and swiftly as possible.
Having different professional perspectives within safeguarding practice is a sign of a healthy and well-functioning partnership. These differences of opinion are usually resolved by discussion and negotiation between the practitioners concerned. It is essential that where differences of opinion arise they do not adversely affect the outcomes for children and young people and are resolved in a constructive and timely manner.
Differences could arise in a number of areas of multi-agency working as well as within single agency working. Differences are most likely to arise in relation to:
- criteria for referrals
- outcomes of assessments
- roles and responsibilities of workers
- service provision
- timeliness of interventions
- information sharing and communication.
If you have difference of opinion with another practitioner, remember:
- professional differences and disagreements can help us find better ways improve outcomes for children, adults and families
- all professionals are responsible for their own cases and their actions in relation to case work
- differences and disagreements should be resolved as simply and quickly as possible, in the first instance by individual practitioners and /or their line managers
- all practitioners should respect the views of others whatever the level of experience – remember that challenging more senior or experienced practitioners can be hard
- expect to be challenged; working together effectively depends on an open approach and honest relationships between agencies
- professional differences are reduced by clarity about roles and responsibilities and the ability to discuss and share problems in networking forums.
Please see our Resolving Professional Differences / Escalation Policy
Supervision, curiosity and understanding families
For many agencies, the use of effective supervision is a means of improving decision-making, accountability, and supporting professional development among practitioners. Supervision is also an opportunity to question and explore an understanding of a case.
Group supervision and Reflective Practice Groups can be even more effective in promoting curiosity and safe uncertainty, as practitioners can use these spaces to think about their own judgments and observations. It also allows teams to learn from one another’s experiences, and the issues considered in one case may have echoes in other workloads.
Tips for practice:
- present alternative hypotheses
- present cases from the child, young person, adult or another family member’s perspective.
Care and activity settings - sensitivity, curiosity and persistence
Care setting practitioners are perhaps best placed to notice how children are because they have contact with the same child on a regular basis. Practitioners can see changes in appearance, behaviour, alertness or appetite and provide a degree of monitoring of the child’s welfare; in effect, they can be the ‘eyes’ for other professionals working with them. This will also apply to volunteers and workers who run groups and clubs for children, young people or adults.
There are many examples of good practice in care staff where alert to concerns and were able to demonstrate professional curiosity and awareness of possible maltreatment and cumulative risk.
Being professionally curious enables practitioners to challenge a child’s vulnerability or risk while maintaining an objective, in a professional and supportive manner. This is not an easy balance.
Domestic Violence & Abuse and professional curiosity
Many Domestic Homicide Reviews and Serious Case Reviews refer to a lack of professional curiosity or respectful uncertainty. Practitioners need to demonstrate a non-discriminatory approach and explore the issues to formulate judgments that translate into effective actions in their dealings with families.
In particular it is vital that professionals understand the complexity of domestic abuse and are curious about what is happening in the child, adult and perpetrator’s life.
Professional curiosity is much more likely to flourish when practitioners:
- are supported by good quality training to help them develop
- have access to good management, support and supervision
- ‘walk in the shoes’ (have empathy) of the child and/or adult to consider the situation from their lived experience
- remain diligent in working with the family and developing the professional relationships to understand what has happened and its impact on all family members
- always try to see all parties separately.
Working with families where there is domestic violence & abuse can be very challenging and practitioners should not take everything they are told at face value. This is particularly so when a victim is not being seen alone and we should also be alert to the following behaviours which should provoke our professional curiosity:
- the victim waits for her/his partner to speak first
- the victim glances at her/his partner each time they speak, checking her/his reaction
- the victim smooths over any conflict
- the suspected perpetrator speaks for most of the time
- the suspected perpetrator sends clear signals to the victim, by eye/body movement, facial expression or verbally, to warn them
- the suspected perpetrator has a range of complaints about the victim, which they do not defend.
If these signals are present, the practitioner should find a way of seeing the suspected victim alone. Practitioners must be mindful to the needs of young people who may be experiencing inequality and/or violence in their relationships. Practitioners, however curious, cannot protect children and adults by working in isolation. Domestic abuse requires a multi-agency response and families and communities also have a vital role to play in protecting children and adults.
Education settings - curiosity and listening
Education staff are perhaps best placed to notice how children and young people are because they have contact with them on an almost daily basis. School staff can see changes – such as in appearance, behaviour, alertness or appetite – and provide a degree of monitoring of the child’s welfare; in effect, they can be the ‘eyes’ for other practitioners working with the young person.
There are many examples of good practice in education where staff were alert to concerns and were able to demonstrate professional curiosity and awareness of possible maltreatment and cumulative risk.
Being professionally curious enables practitioners to challenge parents and explore a child’s vulnerability or risk while maintaining an objective, professional and supportive manner. This is not an easy balance.
It can be difficult for children to express concerns about their own well being, so practitioners have a responsibility to create an environment in which they can do so. Schools should be careful of ‘organisational deafness’ which minimises the chances of really hearing what young people are saying, for example in relation to concerns about their friends.
Professionals (particularly school staff) should be curious and give sufficient credence to occasions when information is shared by young people.
Health practitioners - authoritative practice and professional curiosity
Authoritative practice and professional curiosity are vital in responding to the often highly complex cases that are characteristic of Reviews, where multiple risks and vulnerabilities may extend over considerable periods of time.
An important aspect of authoritative practice is that every practitioner ‘takes responsibility for their role in the safeguarding process’. Authoritative practice needs to be underpinned by a culture of supportive supervision and service leads and managers have a responsibility to foster such cultures and model authoritative practice in their own leadership by:
- encouraging all health practitioners to take responsibility for their role in safeguarding process, while respecting and valuing the role of others
- allowing practitioners to exercise their professional judgement in the light of the circumstances of a particular case
- encouraging a stance of professional curiosity and challenge from a supportive base.
Example: Supporting engagement – moving from Did Not Attend (DNA) to Child Not Brought (CNB)
In a large number of reviews there was evidence of poor engagement with health and social care services. Parents or carers who do not engage present a challenge to practitioners, but this challenge also provides an opportunity for protection.
When working with vulnerable people and families, health practitioners and services should maintain ‘consistent support for the family’ and curiosity and vigilance towards meeting the vulnerable child’s needs – and be persistent in pursuing non-engagement.
Non-compliance may be a parent/carer’s choice, but it is not the vulnerable child’s. Health service administrators and practitioners should treat repeated cancellations and rescheduling of appointments with curiosity and with the same degree of concern as repeated non- attendance. In doing so, it is essential to recognise families’ vulnerabilities and be flexible in accommodating their needs.
A shift away from the term DNA (did not attend) to CNB (child not brought) would help ‘maintain a focus on the child’s ongoing vulnerability and dependence, and the carers’ responsibilities to prioritise the child’s needs’.
Tips for health professionals to Be Curious!
- know who the named professionals are for your area and that you fully understand their roles – promoting good professional practice and providing advice and expertise for fellow professionals
- ensure that safeguarding is addressed within your clinical supervision
- be aware of the relevant Lewisham safeguarding procedures
- be aware of the need to always have ‘professional curiosity’
- be prepared to be both challenged and challenging within your own professional sphere
- ensure you know how to escalate safeguarding concerns.
Police & Criminal Justice Agencies - "don't take things at face value"
Developing and maintaining an open stance of professional curiosity supports police (and other staff) to consider the possibility of maltreatment, and to challenge and explore issues while maintaining an objective and supportive approach.
Given that criminal justice agencies often deal with specific incidents, supervising individual offenders or investigating stand-alone crimes, there is a risk of seeing an individual or a family only through one lens. Protecting children, young people or vulnerable young adults involves understanding their lives and experiences and making professional judgments.
Children, young people are unlikely to readily disclosure abuse or neglect, this means practitioners have to be able to spot the signs and create a suitably safe and trusting listening environment.
There are examples of police and other professionals focusing on offenders behaviours and not their underlying vulnerabilities.
Children or vulnerable young adults repeatedly going missing should trigger police officers’ professional curiosity, it is vital to consider what is motivating their behaviour.
Practitioners and managers need to be curious, to be sceptical, to think critically and systematically but to act compassionately.
Self-Harm & Suicide Ideation in Young People
Introduction
Mental health problems affect around 1 in 10 children and young people. This includes depression, anxiety, and conduct disorder, and are often a direct response to what is happening in their lives.
Self-harm is when someone hurts themselves on purpose and is a way of expressing deep distress, a way of communicating what cannot be put into words, with very difficult feelings that could build up inside. It is not attention seeking behaviour.
Self-Harm is a very common behaviour in young people and affects around one in 12 young people.
Self-harm and Suicidal Ideation Management Protocol
Self-harm and suicidal threats by a child/young person should always be taken seriously and responded to without delay. This is a critical moment to show compassion, patience and understanding to ensure responses are non-judgemental and trauma informed. It is recognised important to apply Think Family approach supporting the family networks who are impacted by the situation. Self-harming is NOT attention seeking behaviour. It is a clear indication of emotional distress, and that support is needed. Self-harm is a way of coping with difficult or overwhelming situations or emotional states.
This self-harm and suicide ideation management protocol is for all staff, managers and volunteers who support children at risk of self-harm or (who) have engaged in acts of self-harming behaviours or threats of suicide. The protocol has been developed in accordance with London Safeguarding Children Procedures, Working Together 2023, learning from Local Child Safeguarding Practice Reviews, and NHS NICE Guidance.
A summary of the full protocol is available here.
Warning signs of Self-Harm
- People who self-harm may suffer mood swings and become withdrawn.
- Unexplained wounds.
- Have a lack of motivation.
- There may be changes in their eating habits.
- They may cover up their body (even in warm weather).
Warning signs of Suicide Ideation
They may be:
- Quiet, brooding, or withdrawn.
- Feeling exhausted and distant.
- Feeling cut off from those around them.
- Not making eye contact.
- Agitated, irritable or rude.
- Talking about suicide or saying it’s all hopeless.
- Desperate for help but afraid to ask.
They may also:
- Be busy, chirpy, laughing and joking, talking about future plans, and telling you not to worry about them.
The safest way to know if someone is thinking about suicide is to ask them. If a person is suicidal the idea is already there. If they aren’t suicidal it won’t do any harm. Saying something is safer than saying nothing.
Risk Factors of Self-Harm & Suicide Ideation
- Stressful life events.
- Isolation.
- Low self-esteem.
- On-going family relationship problems.
- Being bullied at school.
- Bereavement.
- Mental health problems – depression and delusional thoughts.
- Substance and alcohol misuse.
- Family circumstances.
- Stress and worry – academic pressure.
- Experience of abuse – physical, emotional, sexual abuse, sexual exploitation, and forced marriage.
- Feelings of being rejected in their lives.
Types of Self-Harm
- Cutting of the skin with objects (e.g. razor blades, scissors, pens, bottle tops etc.)
- Scratching the skin.
- Picking wounds or interfering with healing.
- Burning.
- Ingesting toxic substances.
- Excessive drug or alcohol intake.
- Hitting or punching themselves.
- Head banging or biting themselves.
- Pulling hair out.
- Swallowing or inserting objects.
- Taking an overdose.
- Staying in an abusive relationship.
- Taking risks too easily.
- Restricting their eating. Young people can self-harm in a variety of body locations, i.e. arms, legs, abdomen, etc.
Responding to Self-Harm in Lewisham +
If a child or young person overdoses or there is a serious self-harm incidence they should be taken to A&E in the first instance. An assessment will be undertaken which may involve a referral to the Children & Adolescent Mental Health Service (CAMHS).
If you become aware of a young person who is self-harming or having suicidal thoughts. Explore their feelings with them and talk about the help available:-
Share what you know with the child’s parents / carers.

Tips for Talking with Young People - Print The Poster!
Services +
Young Minds
- Parents Helpline 0808 802 55 44
- Advice for professionals
GP
- Ask the parent / carer to make an appointment.
CAMHS
Kooth
- Online chat support for young people
Papyrus Hopeline 0800 068 41 41
- Confidential advice for young people
- Advice for parents / carers.
- Advice for professionals
ChildLine – 0800 11 11
- Confidential advice for young people
- Advice for professionals
Place2Be
- Individual one to one, drop in counselling for children and young people experiencing emotional wellbeing issues at 10 schools in Lewisham
National Self-Harm Network
- UK charity offering moderated support forum for self-harm
NHS Choices - Moodzone
- Online and audio resources to improve mental wellbeing and information about available treatments
MindEd
- Online training for anyone working with 0-18 year olds
Resources
Coping with Self-Harm, A Guide for Parents & Carers
Calm Harm App.
Down load this from your AppStore or GooglePlay. The app offers activities to comfort, distract, express yourself, Release, Random and Breathe.
Signs of Safety Practice Framework

Introduction
In Lewisham we use the Signs of Safety practice framework across the whole of children’s services in our work with children and families. We use this model because it helps Professionals and families to think through problems and solutions together rather than families feeling that everything is being dictated to or done for them.
No matter how difficult a family’s situation there will always be existing strengths, resources and abilities they can draw on; the Signs of Safety approach helps professionals to help families and children identify and build on these existing resources for themselves.
The Signs of Safety assessment and planning process is designed to bring professionals and families together using four core questions:
- What are we worried about?
- What’s working well?
- What needs to happen?
- Where would you rate things for the child on a scale of 0 to 10 where ten means the child is safe and professionals can close the case and 0 means the situation is dangerous for the child and they very likely need to live away from their parents until things change?
Partner Briefings
To familiarise partners with Signs of Safety we provide regular half day briefings, the aim of which is:-
- To develop an understanding of the Signs of Safety principles and practice framework and how it is applied within Children’s Services
- To gain a working knowledge of the Signs of Safety mapping assessment framework
- How to use the framework to make effective contributions to multi-agency meetings such as child protection conferences and Child in need Reviews/Core Groups
- Writing pre-conference reports or making referrals to MASH using the mapping framework
- Supporting the process of safety planning with the family and network
- Ensuring the voice of the child and their lived experience is heard/understood
- The skilful use of authority and maintaining positive working relationship with family and professionals
To View and Book please follow this link: https://www.safeguardinglewisham.org.uk/events/event/signs-of-safety-partnership-briefing
Signs of Safety Toolkit
The following tools include:
1-4: Templates for the mapping assessment framework for Signs of Safety/Aspiration/Success/Wellbeing with prompt questions.
1. Mapping Framework Guide and Prompt Questions
2. Signs of Aspiration of Success Mapping Framework Guide with Prompt Questions
3. Signs of Wellbeing Mapping Framework Guide and Prompt Questions
4. SoS Mapping Framework including Contextual Factors and Questions
5&6: A guide and Template for using the My Three Houses tool for gathering information from a child.
5. My 3 Houses Templates
6. My 3 Houses Practice Guidance.
7: The Harm Matrix tool which provides questions to help you unpick your worries around a child and identify exactly what the harm they are suffering looks like and how worrying it is.
7. Harm Matrix Tool
For more information
A short video introducing Signs of Safety by one of its creators – Andrew Turnell
Web site: https://www.signsofsafety.net/
For further advice or consultation
Alex Campbell alex.campbell@lewisham.gov.uk
Signs of Safety Practice Lead, Lewisham Workforce Development Team
Think Family Approach
In April 2023, Lewisham Safeguarding Children Partnership (LSCP) and the Lewisham Safeguarding Adults Board (LSAB) and jointly agreed to focus on Think Family as a strategic priority.
Learning from Local Child Safeguarding Practice Reviews and Safeguarding Adults Reviews have highlighted the importance of adult and children’s services working collaboratively and taking a joined up, whole family approach.
Families are dynamic, evolving and not linear. When we describe family, we mean:
Anyone who is identified by the service user as their family or who is part of their family network.
In Lewisham we have identified that a Think Family approach highlights:
- The importance of practitioners thinking about children and adults’ the wider context.
- The need to focus on family networks which safeguard and provide nurture and care for children and adults.
- The importance of looking beyond the household, to consider their extended family, friends, and the community.
- The importance of recognising children and adults’ connectedness to wider contexts than your immediate family, this could include faith leaders, mentors, and community support.
Familiarise
Familiarise yourself with the family, their unique culture, character, strengths and vulnerabilities. Who are the significant people in their lives (including any new partners/adults in the home)?
Ask
Be professionally curious about everything and ensure that when you encounter a family that you physically check that everyone in the household is safe and well.
Make a Plan and Review
Decide what actions you need to safeguard ‘adults at risk’ or children. Give special consideration to people who are pregnant and unpaid carers, and particularly young carers.
Information sharing
Information gathering and sharing is key to building a Think Family approach. Do not assume someone else knows an important piece of information.
Liaise
To demonstrate collaborative working, practitioners must communicate effectively to share concerns and work holistically together.
Your Responsibility
We must take responsibility for ensuring that we work effectively with our partners to help support families, and in doing so prevent abuse and harm.
Engaging Families
How we engage with families, children and young people is a critical skill to support positive engagement, participation and collaboration with families. Learning from reviews in Lewisham has highlighted a need for professionals to consider their approach to engaging families to ensure families receive intervention and support from the right service at the right time.
Engaging families can present challenges resulting in some families not receiving the necessary services to ensure the safety of their child/ren and themselves. There can be many factors contributing to why families may struggle to access support services, and professionals need to approach this with curiosity, compassion, and a trauma-informed perspective while prioritising the well-being of the children in decision-making.
This guidance aims to help staff, whatever their role, to understand the barriers to engagement and provide strategies to creatively engage children, young people, and their families.
Working with Fathers and Carers Toolkit
The toolkit provides practical strategies for engaging fathers and male carers in early help and social work, recognizing their significant impact on children's development and family outcomes.
Research Insights:
Engaging fathers in early help and social work has been shown to positively impact children in several areas:
- Improved Educational Attainment: Better school performance.
- Enhanced Cognitive Development: Improved thinking and problem-solving skills.
- Better Emotion Regulation: More effective emotional management.
- Positive Behavioural Effects: Overall behavioural improvements.
- Improved Social Competence: Better interactions with peers and adults.
- Higher Self-Esteem: Increased confidence and self-worth.
Tools for Supporting Dads and Male Carers:
- Element 1 - Think About Dads and Male Carers: Consider dads and male carers in inclusive and positive work with families.
- Element 2 - Promote to Dads: Actively promote services and support to fathers.
- Element 3 - Engage with Dads: Develop strategies to effectively engage fathers.
- Element 4 - Work with Dads: Collaborate with fathers in providing support and services.
- Element 5 - Motivate Dads: Encourage and motivate fathers to participate actively.
- Element 6 - Learn More About Working with Dads: Continuously improve understanding and skills for working with fathers.
Young Carers
Imago is a charity that supports local communities. One of the groups that they support is carers. They support over 12,000 carers through services, including over 8,000 young carers from the age of 4, young adult carers and adult carers.
Imago offers the Maximising Wellbeing for Unpaid Carers service to young carers in Lewisham that are taking on caring responsibilities for a family member with a long-term illness, disability, mental health or substance misuse issue. Young Carers support the cared-for and other family members with practical tasks, physical care, and emotional support, whilst at the same time trying to live their own lives. They support young carers in Lewisham to minimise the negative impacts of caring and to access social and educational opportunities and emotional support, highlighting the positive impacts of being a carer, such as increased resilience and empathy.
Young carers can access a variety of activities, workshops and respite trips. The service also includes one-to-one support and in school support when needed. Working alongside school staff and other professionals, they aim to ensure young carers have access to the support they need and know they are not alone.
The Maximising Wellbeing for Unpaid Carers service works with schools, communities, and statutory and voluntary agencies to identify hidden Young Carers and offers training and information to professionals.
To complete an online referral go to https://www.imago.community/Carers/lewishamcarers
For more information contact the hub on 0300 373 5769 or email ucwellbeing@imago.community.